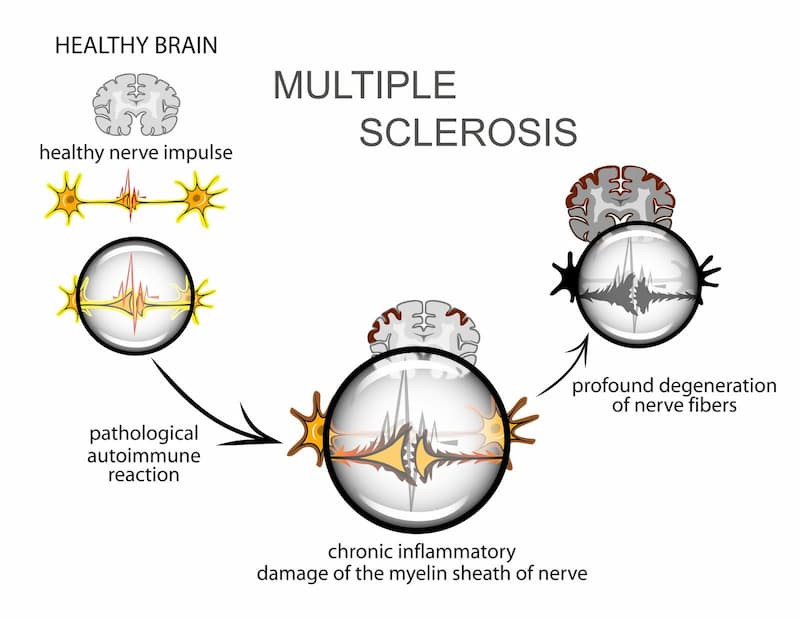
Multiple sclerosis is a chronic degenerative condition that occurs as a result of the faulty response of the immune system. It is an autoimmune condition, which means it develops when the immune system fails to identify the body’s own tissues as ‘self’ and mounts an attack destroying healthy tissues. Specifically, it targets the protective myelin sheath that surrounds nerve fibers in the brain and spinal cord. This damage disrupts the communication between the brain and the rest of the body, leading to a wide range of neurological symptoms. Over time, the destruction of myelin and nerve fibers can result in permanent damage and a decline in physical and cognitive abilities.
There are different types of MS, depending on the stage of the disease and symptoms. Recent research suggests that stem cell therapy could be effective in the management of these types of multiple sclerosis.
This article discusses the main types of this condition among different types of MS and provides information on whether stem cell therapy can help in the management of this condition.
How Many Types of Multiple Sclerosis Are There?
Multiple sclerosis is a gradually progressive degenerative condition. It occurs when the immune system attacks and destroys the tissues of the nervous system. It specifically affects the myelin sheath covering the nerves, due to which the transmission of signals through the nerve fibers is hampered.
If not treated properly, multiple sclerosis can progress over a period even worse, resulting in significant damage to the nervous system. Although the body attempts to heal the nerves and myelin sheath, the nerve damage may progress until symptoms become permanent or long-lasting.
There are 4 types of MS, which are considered the most common:
- RRMS (Relapsing-remitting MS)
- SPMS (Secondary progressive MS)
- PPMS (Primary progressive MS)
- PRMS (Progressive-relapsing MS)
Here is a brief explanation of the symptoms associated with these 4 multiple sclerosis types.
Review of the 4 types of MS
The 4 types of multiple sclerosis reflect the progressive nature of this condition. Being aware of the early warning signs of multiple sclerosis can help patients seek timely medical intervention and delay potential complications.
Here is a review of the different types of MS and what happens at each stage of this condition.
Relapsing-Remitting MS (RRMS): The Most Common Form
Relapsing-remitting MS is the most common among the 4 types of multiple sclerosis. Most patients diagnosed with multiple sclerosis have this phenotype of nerve damage.
RRMS is characterized by periods of relapse and remission. During periods of relapse or acute attacks, patients develop neurological symptoms, such as pain, tingling, and numbness along the course of the nerve. These symptoms persist for a variable duration, followed by a period of remission when the symptoms subside fully or partially.
Many patients with RRMS recover substantially or fully after each episode of relapse. However, each patient comes with a unique set of symptoms and patterns of remissions and relapses, which can make it challenging for the doctor to prescribe the most appropriate treatment. Yet, an early diagnosis can offer a more efficient way for patients with relapsing-remitting MS to overcome their symptoms and live healthy and active lives.
Secondary Progressive MS (SPMS): Transitioning From RRMS
Secondary progressive MS marks the transition from the RRMS stage of this disease. SPMS is characterized by constant deterioration of the condition without remission.
SPMS may be ‘active’ or ‘not active’. It may also be classified as ‘with progression’ or ‘without progression’. These disease modifier terms are used to describe the severity or extent of the progression of the disease and the frequency and duration of relapses and remissions.
Primary Progressive MS (PPMS): Gradual Worsening Without Relapses
The diagnosis of primary progressive MS signifies gradual worsening of nerve damage without relapses. This is the rarest form of multiple sclerosis diagnosed in 10 to 15% of patients with this condition.
The clinical diagnosis involves the assessment of the symptoms and their impact on the patient’s routine activities and quality of life. Modifiers such as ‘active’, ‘not active’, ‘with progression’, and ‘without progression’ are used to describe the disease activity.
PPMS develops when patients with multiple sclerosis experience a constant progressive deterioration without remissions.
The treatment of PPMS is challenging due to the increase in the extent of nerve damage. It often results in a higher level of disability, which increases the risk of dependency for the patient. Most patients with PPMS require assistance to complete their daily activities.
Progressive-Relapsing MS (PRMS): A Rare And Aggressive Type
Progressive-relapsing MS is one of the most rare and aggressive multiple sclerosis types that affects only a very small percentage of patients.
It is the worst type of MS that progresses steadily from the onset of the first symptoms and is interspersed with variable periods of relapses and remissions. This form of MS is characterized by a continuous worsening of neurological function from the very beginning, with no clear periods of recovery. Patients with progressive-relapsing MS often experience significant disability and a rapid decline in life quality, making it one of the most challenging forms of the disease to manage.
Get a free online consultation
Please, contact our medical advisor to discuss your health condition with a specialist in regenerative medicine. You can also leave your contact details for a callback. It is free and confidential.

Medical Advisor, Swiss Medica doctor
Comparing the 4 Forms of MS: Key Differences and Symptoms
The 4 types of MS indicate the stage of the disease. This helps assess the extent of nerve damage and disability, so healthcare practitioners could recommend the most appropriate treatment.
Also, there is no clear-cut demarcation between multiple sclerosis types. Rather, there is considerable overlap between these stages of multiple sclerosis, and it is difficult to determine when the patient progresses from one stage to the next.
Initially, most patients with these types of MS experience neurological symptoms of varying intensities. The episodes of symptom occurrences are called relapses, attacks, or exacerbations. During the episodes of relapse, the patient is likely to have new symptoms or experience worsening of the existing symptoms.
The period of relapse usually persists from a few days to a few months in the relapsing-remitting stage of the disease. Over a period, RRMS might advance to SPMS. This form of multiple symptoms does not exhibit dramatic variations in symptoms or disability compared to RRMS. It rather indicates a slow, steady progression of nerve damage.
Patients with active SPMS may initially experience relapses, although these usually do not subside fully. Without treatment, patients experience continued progression of disability without any relapses. This is referred to as “non-active” SPMS.
It is estimated that, in the absence of proper treatment, approximately 50% of patients with RRMS develop the worst type of MS, such as PPMS within 10 years. However, with the introduction of advanced disease-modifying therapies, such as stem cell treatments, the progress to PPMS can slow down to a great extent.
In addition, stem cell therapy may also lower the frequency and duration of relapse and increase the duration of remission in patients even with the most advanced types of MS, including PPMS and PRMS.
Diagnosing Multiple Sclerosis: Tests and Procedures
There are no specific tests for the diagnosis of types of MS. Hence, the diagnosis is usually made based on the typical symptoms associated with nerve damage, after eliminating other conditions that are likely to produce similar symptoms.
The complete medical history of the patient and physical examination can often help to point to the possible diagnosis of multiple sclerosis. The doctor might recommend additional tests to evaluate your case further to get the probable diagnosis of this condition.
Your doctor might recommend the following tests as a part of the assessment of different types of multiple sclerosis:
- MRI, which may reveal areas of abnormal lesions in the brain, or thoracic and cervical spinal cord associated with different types of multiple sclerosis.
- Spinal tap, also called lumbar puncture. It is a procedure in which a small sample of cerebrospinal fluid is removed from the spinal canal and tested in a laboratory to check for the presence of antibodies associated with MS.
Living with MS: Treatment Options and Lifestyle Tips
Currently, there is no cure for multiple sclerosis. The treatment of this condition is typically focused on relieving the symptoms and supporting recovery from acute attacks. The treatment also includes medication and lifestyle changes to prolong the periods of remission.
The prognosis of patients with multiple sclerosis type of disease depends on the stage of nerve damage. Several factors, including the age of onset of the disease, the patient’s gender, the severity of symptoms, the extent of disability, and the response to the treatment, can affect the treatment outcomes and progression.
Regardless, living an active and fulfilling life with different forms of MS can be possible by eating a nutritious diet, maintaining a healthy lifestyle, focusing on symptom management, and seeking appropriate medical care.
Living with the worst type of MS can become less challenging and more fulfilling by choosing healthy lifestyle strategies such as:
- Eating a balanced diet
- Getting adequate rest
- Regular exercise
- Avoiding exposure to extreme heat
- Adopting stress-relieving strategies such as yoga, meditation, and deep breathing exercises
Stem Cell Research for Multiple Sclerosis
Stem cell research on multiple sclerosis type of disease has revealed promising findings. Clinical research suggests that the administration of stem cells can help with CNS lesions, recover neurological deficits, and cause immunomodulatory effects in some of the 4 types of MS.
Types of stem cells being researched include:
- Mesenchymal Stem Cells (MSCs): These cells, derived from bone marrow, adipose tissue, or umbilical cord tissue, can produce immunomodulatory and anti-inflammatory properties, reducing immune system attacks on myelin and promoting tissue repair.
- Hematopoietic Stem Cells (HSCs): These cells can be found in bone marrow and peripheral blood. HSCs may reset the immune system by destroying existing immune cells and creating new ones from the transplanted stem cells. This can potentially halt disease progression and reduce relapses.
- Neural Stem Cells (NSCs): This type of cells can be derived from embryonic stem cells or created from induced pluripotent stem cells (iPSCs) or adult somatic cells. NSCs have potential for repairing damaged myelin and restoring nerve function.
- Induced Pluripotent Stem Cells (iPSCs): These cells are generated by reprogramming adult cells, such as skin cells, to an embryonic-like state. As iPSCs can potentially differentiate into any cell type, they can become oligodendrocytes responsible for myelin production.
Key research areas include:
- Immune modulation: Using MSCs and HSCT to reduce the autoimmune response and prevent further damage of myelin.
- Myelin repair: Using NSCs and iPSCs to generate new myelin-producing cells and restore nerve function.
- Neuroprotection: Exploring the neuroprotective properties of various stem cells to preserve nerve function and protect neurons from ongoing damage.
Current clinical trials and studies are also investigating the long-term safety and efficacy of stem cells, as well as determining the most effective types of stem cells and delivery methods. Doing research is important as it makes stem cell therapies more accessible to patients, considering factors such as cost, availability, and regulatory approval.
Multiple Sclerosis Treatment with Stem Cells
Stem cell therapy may improve the prognosis of different forms of multiple sclerosis by supporting the regeneration of new nerve cells and inhibiting the autoimmune repose of the nervous system.
Stem cells possess various beneficial properties:
- Anti-inflammatory: The anti-inflammatory properties of mesenchymal stem cells can reduce inflammation in the nerves and minimize damage to the myelin sheath.
- Regenerative: Stem cells administered into the body of the patients support the regeneration of new healthy cells. These cells can differentiate to form specialized cells that make up the nerves and myelin sheath. The cells can replace the damaged cells, thereby restoring the structural and functional integrity of the nervous system.
- Immunomodulatory: These properties can modify the response of the immune system and inhibit the self-destructive activity of the immune system against the body’s healthy tissues, such as the nerves.
Some evidence suggests that treatment with stem cells in patients with MS may:
- Regulate the immune system;
- Reduce inflammation in certain types of MS, such as active relapsing and active progressive MS;
- Slow down the progression of MS;
- Decrease the number of new lesions and relapses;
- Alleviate MS symptoms.
Patients diagnosed with multiple sclerosis can consult our stem cell experts at Swiss Medica Clinic to learn more about stem cell research on multiple sclerosis and whether this treatment could be effective for managing their condition.
Importance of Early Diagnosis and Management of Multiple Sclerosis
Early diagnosis of 4 types of multiple sclerosis plays a crucial role in the management of this condition as it allows patients to seek timely medical interventions. It also helps them make appropriate changes in their diet and lifestyle to slow down the progression of nerve damage.
Being aware of the early warning signs of multiple sclerosis can be helpful for getting an early diagnosis. Patients who experience any signs of multiple sclerosis can consult our stem cell experts at Swiss Medica Clinic for a careful evaluation of their health issues.

Our doctors will analyze your symptoms, medical history, and family history and recommend the best possible treatment for managing your condition.
Conclusion
Multiple sclerosis is a chronic progressive autoimmune condition, which can create a significant negative impact on the patient’s routine life. The disease is characterized by the immune system mistakenly attacking the myelin sheath that protects nerve fibers, resulting in inflammation and damage to the central nervous system. There are 4 forms of multiple sclerosis: clinically isolated syndrome (CIS), relapsing-remitting MS (RRMS), primary progressive MS (PPMS), and secondary progressive MS (SPMS). Each type presents unique challenges and progression patterns. Early diagnosis and timely medical intervention of 4 types of multiple sclerosis can improve the prognosis and ease the patient’s life to a great extent.
Prompt treatment can help modulate the immune system, reduce inflammation, and slow disease progression. It can also diminish the number of new lesions and relapses, ultimately improving the patient’s quality of life.
Ongoing research and advances in stem cell therapies offer hope for more effective treatments. These therapies aim to repair damaged tissues, regulate immune responses, and potentially restore lost functions, providing a promising outlook for those living with MS. With continued scientific progress, the management of MS is expected to improve, offering better therapy results and enhanced quality of life for patients.
Contact us
Get a free online consultation to learn about the expected results of stem cell therapy for your case, what is the cost of the treatment, and its duration.

Medical Advisor, Swiss Medica doctor
List of References
Tafti, D., Ehsan, M., & Xixis, K. L. (2024). Multiple Sclerosis. In StatPearls. StatPearls Publishing.
Ghasemi, N., Razavi, S., & Nikzad, E. (2017). Multiple Sclerosis: Pathogenesis, Symptoms, Diagnoses and Cell-Based Therapy. Cell journal, 19(1), 1–10. https://doi.org/10.22074/cellj.2016.4867
Steinman L. (2014). Immunology of relapse and remission in multiple sclerosis. Annual review of immunology, 32, 257–281. https://doi.org/10.1146/annurev-immunol-032713-120227
Inojosa, H., Proschmann, U., Akgün, K., & Ziemssen, T. (2021). A focus on secondary progressive multiple sclerosis (SPMS): challenges in diagnosis and definition. Journal of neurology, 268(4), 1210–1221. https://doi.org/10.1007/s00415-019-09489-5
Thompson A. (2004). Overview of primary progressive multiple sclerosis (PPMS): similarities and differences from other forms of MS, diagnostic criteria, pros and cons of progressive diagnosis. Multiple sclerosis (Houndmills, Basingstoke, England), 10 Suppl 1, S2–S7. https://doi.org/10.1191/1352458504ms1024oa
Tullman, M. J., Oshinsky, R. J., Lublin, F. D., & Cutter, G. R. (2004). Clinical characteristics of progressive relapsing multiple sclerosis. Multiple sclerosis (Houndmills, Basingstoke, England), 10(4), 451–454. https://doi.org/10.1191/1352458504ms1059oa
Lemus, H. N., Warrington, A. E., & Rodriguez, M. (2018). Multiple Sclerosis: Mechanisms of Disease and Strategies for Myelin and Axonal Repair. Neurologic clinics, 36(1), 1–11. https://doi.org/10.1016/j.ncl.2017.08.002
Genc B, Bozan HR, Genc S, Genc K. Stem Cell Therapy for Multiple Sclerosis. Adv Exp Med Biol. 2019;1084:145-174. doi: 10.1007/5584_2018_247. PMID: 30039439.
Stem cell therapy for MS. 2024. https://www.msif.org/research/challenges-of-ms-research/stem-cell-therapy-for-ms/?cn-reloaded=1
MD, Pediatrician, Regenerative Medicine Specialist







