Stem cells hold a great promise to treat brain injury with their unparalleled regenerative properties. More than symptom management, stem cell therapy for brain injury actually helps repair damaged brain tissue and promotes neurogenesis (the growth of new neurons).
Find out in this guide how stem cell therapy works, who this type of therapy may benefit, and why this is a hope for people with traumatic brain injuries. Learn about brain stem cell treatment costs, treatment options, and the potential this advanced treatment holds.
Why the Use of Stem Cells is the Future of Treatment for Brain Injuries?
Can stem cells repair brain damage? Stem cell treatment for brain injury may contribute to:
- Various research has documented that the therapeutic approach with stem cells can improve cognitive function, the ability to move, quality of life, and reduction of inflammation in brain injury patients treated with stem cells.
- The unique capacity for the regeneration of injured brain tissue belongs to the following kinds of cells: stem cells, including neural stem cells and mesenchymal stem cells.
- Stem cells secrete neurotrophic factors that would protect the existing neurons and facilitate the survival of the brain cells, thus allowing lesser damage following an injury.
- With stem cells, the future prospect of personalized medicine might come true. This would, in turn, render the treatments far more effective and widely available to people in general.
Stem cells for brain repair, coupled with these regenerative capabilities, holds great promise for the treatment of brain injuries and is hope for long-lasting recovery.
Types of Brain Injuries That Can Be Treated With Stem Cell Therapy
Apart from the treatment of brain trauma associated with various pathologies, stem cell therapy for brain damage can also benefit different conditions within the human body, including:
Traumatic Brain Injury (TBI)
The most common cause of TBI is an accident and head trauma. Patients suffering from TBI may find stem cell therapy for traumatic brain injury effective, as it helps reduce inflammation in the injured brain and promote regeneration of neurons and other cells of the brain-damaged area. They also secrete neurotrophic factors, which support neuroprotection and the regeneration of the brain. In clinical tests, MSC treatments enhanced neurological functions and regained consciousness in patients suffering from TBI. Stem cell treatment might result in less inflammation and a restoration of neurological functions, which could give way to the improvement of cognitive and motor skills.
Stroke-Damaged Brain
In brain injuries resulting from stroke, partial death of the brain tissue occurs due to inadequately supplied blood flow. The primary positive aspect of stem cell therapy for brain damage is that it can bring back lost function by neurogenesis (formation of neurons) and angiogenesis (formation of new blood vessels). Restoration of damaged neurons and improvement in blood flow aid in promoting recovery. MSCs transplantation following strokes in many pre-clinical studies helped reduce sizes of infarctions and, hence, improve the outcomes in the long run.
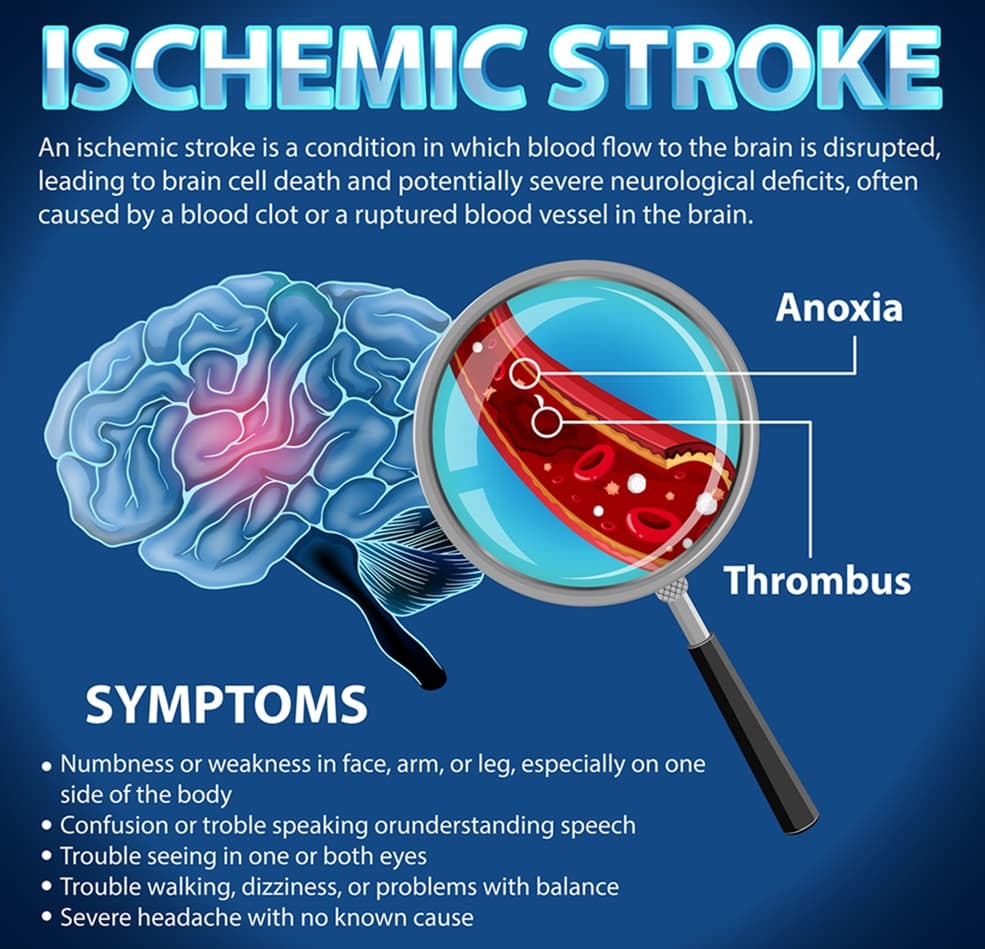
Hypoxic-Ischemic Brain Injury
Near-drowning and birth complications are the usual causes of brain injuries. Hypoxia and ischemia are causes of this kind of brain injury. Stem cell transplant for brain damage promotes regeneration of damaged brain tissue and minimizes long-term neurological deficits by means of growth factors, protection of the blood-brain barrier, and the release of exosomes.
Stem Cell Therapy and Its Capability to Help With Brain Injuries
Can stem cell therapy help brain damage? For years, it has gained much attention for its regenerative potential. The two types of stem cell therapies relating to traumatic brain injuries are mesenchymal stem cells and neural stem cells. Here is a look at how stem cell therapy for brain injury can be helpful.
- Stem cells for brain injury have the potential to regenerate tissue by proliferating into the different types of brain cells that will aid in repairing the damaged portion of the brain. Because these cells release growth factors, they can also promote the inherent healing capability of the brain by stimulating nearby cells, thus creating an environment in the brain that is conducive to healing.
- Neurons may be destroyed by inflammation and oxidative stress, but protective factors released by them prevent further destruction.
- Another important role of stem cells is the modulation of the immune response. This helps reduce the inflammation, which is one of the prime causes of continued damage subsequent to a brain injury.
- Stem cell treatment for brain injury fosters neovascularization, or the formation of new blood vessels, thus improving blood flow and oxygenation of injured brain tissue to promote its healing.
- The stem cells trigger neuroplasticity. It causes the reorganization of the brain and hence enhances the cognitive, motor, and sensory capabilities.
Stem cell therapy is a potentially effective treatment for brain injury as it deals with its acute phase and its long-term consequences.
Get a free online consultation
Contact us to learn about the expected results of the treatment, its cost and duration.

Medical Advisor, Swiss Medica doctor
Benefits of Stem Cell Therapy for Brain Damage
Efficiency and Non-invasiveness
Many of these therapies with stem cells can employ delivery methods that are minimally invasive, such as intravenous injections or intrathecal delivery. This greatly reduces the necessity for complicated surgeries. Patients with traumatic brain injuries are able to recover sooner and have fewer risks associated with the more invasive procedures.
A lower risk of side effects compared to conventional treatments
Stem cell therapy for brain injury has fewer side effects compared to conventional treatments, which involve surgery or medications. Because the therapy makes use of the body’s natural healing mechanism, infections, immuno-reactions, and drug reactions are rare.
Positive Clinical Outcomes Based on Research
MSCs have been utilized in clinical trials to promote improvement in brain functionality, reduce inflammation, and increase neurogenesis. There was also noticeable improvement in the motor functions and cognitive capabilities of patients with MSC therapy compared to the control groups. Stem cells for brain injuries are under constant research, and the active trials support the potential effectiveness of the stem cell treatment.
Personalized Approach
This is personalized treatment wherein various types of stem cells, routes, and timing can be used depending on the specific needs of each patient. The patients might receive multiple treatments with various types of stem cells, various routes of administration, and different times. The personalized approach of stem cell treatment for brain injury helps to increase the chances of success, wherein the progress of every patient is constantly monitored.
Stem Cell Therapy Procedure: What to Expect
How are stem cells used to treat brain damage? The answer involves some explanation of the phases of the treatment.
- During the consultation, the doctor determines whether the patient is a good candidate for the application of stem cell therapy and the type of stem cells to be used. This would involve a review of the patient’s medical history, physical and neurological exams, and possibly the carrying out of imaging studies (e.g., MRI, CT scan).
- After assessment, doctors come up with an individualized program regarding stem cell therapy for brain injury. It denotes which type of cells will be used—for example, mesenchymal stem cells or neural stem cells—the route of administration, and the number of sessions of treatment a patient needs to take to receive the best results.
- It is possible to collect stem cells either from the recipient’s body, also called an autologous collection, or from another donor, thus being allogeneic. If autologous stem cells are used, a procedure in the bone marrow or, alternatively, in the adipose tissue has to be performed to collect them. Allogeneic cells, if used, are obtained through extensive processing and screening for their safety.
- After being harvested from the body, the stem cells are separated and concentrated in a specialized lab. Filtration, centrifugation, or other techniques help create concentrated cells. In addition, the cells will have to be prepared in such a way that they will be free of all impurities and are ready for use in therapy by ensuring that they are pure, viable, and suitable.
- Depending on the condition and the patient, physicians administer stem cells for brain repair through intravenous infusions or intrathecal administration. It lets the stem cells circulate in the blood and reach the damaged areas, while targeted injections allow treating the specific areas with more effectiveness.
- The doctor then follows up on the patient post-procedure to ensure that there are no immediate complications. Follow-ups serve to monitor the progress of the patient and assess the effectiveness of the treatment provided. A combination of physiotherapy and occupation therapy can achieve maximum recovery after the administration of stem cells.
- In the long run, doctors would observe the patient’s progress in weeks and months to come since the stem cells are working their ways to repair and regenerate the damaged tissue. Long-term follow-up care is usually used for patients to prevent complications that may arise late and schedule repeated treatments.
Stem cell therapy for brain injury has nuances based on the patient’s condition and type of stem cells in use. However, this brief description encompasses major steps of treatment using stem cells.
Risks and side effects of stem cell therapy for brain injuries
Generally, stem cell treatment is safe, though there are some possible side effects:
- Fatigue
- Headache
- Chills
- Nausea
- Low-grade fever
- Pain or discomfort related to an injection
- Redness, Swelling, or Bruising
These side effects are usually mild and temporary and get resolved within days.
By far, the most significant risk comes from unregulated clinics or practitioners offering stem cell treatments. To ensure safety for patients, treatment with stem cell transplants for brain injury should be performed in licensed, credible medical facilities only.
Best Stem Cell Therapy for Brain Damage
In general, the effectiveness of stem cell therapy for brain damage depends on the variety of stem cells applied, the mode of administration of such cells, and the pathology being addressed. Some of the most promising options of treatments using stem cells for brain damage include:
- Mesenchymal stem cells (MSCs) are one of the most common types of brain stem cell treatment because they enhance neuronal survival through the secretion of neurotrophic factors and reduce inflammation, hence protecting the brain tissue. The role of MSCs in the regulation of the immune response within the injured brain decreases inflammation and improves the pace of healing. The source for stem cells includes the use of bone marrow, adipose tissues, and umbilical cord tissues.
- Neural stem cells (NSCs) are a subcategory of stem cells that have the potential to differentiate into neurons or glial cells capable of replacing function within the body. They therefore hold particular promise for strokes, traumatic brain injuries, and neurodegenerative diseases because they can actually regenerate neural tissue. NSCs are usually derived in the laboratory from bone marrow MSCs.
- The exosome treatment involves the use of nanosized extracellular vesicles, for example, those secreted by MSCs in treating a variety of sickness or disease states. However, exosomes are not stem cells, but their role is to facilitate inter-cellular communication and promote tissue repair. By improving the survival of cells and aiding the recovery of neurons, exosomes may enhance cell survival and promote neuronal recovery. Anti-inflammatory properties of these agents reduce neuroinflammation due to brain injuries.
Success with stem cell therapy depends on specific factors such as a patient’s physical condition and the severity of the injury. Mesenchymal and neural stem cells for brain injury hold immense promise for modulating the damaged brain environment. Newer treatments, including exosome therapy, hold even more tailored approaches.
The Best Stem Cell Clinic for Brain Injury Treatment
Choosing the right stem cell therapy clinic is highly important for better recovery from any kind of brain injury. While selecting a stem cell clinic, consider a few of these things:
- Consider clinics with highly qualified and experienced professionals, especially if treatment for a brain injury is needed.
- Leading clinics offer a range of cell options with delivery methods using modern techniques and, therefore, far better outcomes because the stem cells actually reach the damaged brain areas. Clinics with their own labs or those partnered with advanced cell processing facilities ensure that the utilized stem cells are pure, viable, and safe.
- You need to collect reviews and testimonials from patients to get an idea concerning the effectiveness of treatments.
If you are considering the use of stem cell therapy to treat brain damage, the experts at Swiss Medica are here to help. Advanced stem cell treatments in our practice, individually designed for specific patient needs, offer symptom alleviation and overall health improvements.
A no-obligation assessment with Swiss Medica medical professionals will allow you to discuss your individual condition and the possibility of applying stem cell therapy. This consultation is going to try to answer the question, ‘Can stem cells help with brain damage?’
Everything from how the stem cells may relieve inflammation and regenerate damaged tissue to what you can expect of the therapy is discussed herein. We try to provide all the information one needs to make an informed choice about the treatment.
How Swiss Medica Can Help You Recover From Brain Injury Using Stem Cells?
Choosing Swiss Medica Clinic for stem cell therapy for brain damage offers the following advantages:
- You are welcome to schedule a no-obligation consultation before commencing your treatment to answer your questions, explain doubts, and explain the procedure.
- Each patient has an individual plan of treatment depending on his case and the goal of his treatment to get the best results for him.
- We are located in Serbia, which is easily accessible through direct flights from major cities and countries.
- We retain the services of a team of doctors and medical staff with expertise in regenerative medicine and years of experience performing up-to-date stem cell treatments.
- Modern state-of-the-art medical facilities within the clinic ensure comfort, safety, and efficiency during treatment.
- The comprehensive travel assistance takes in accommodation, airport transfers, and continuous medical consultations.
- Follow-up and follow-through care and monitoring are very important aspects of our services to ensure long-term success.
- At every point in one’s treatment with us, we adhere to extensive quality control standards to ensure the vitality, purity, and safety of the cells.
- The lab’s location right at the clinic ensures proper dosing and preparation of the stem cells to achieve maximum results.
- This wide range of stem cell types and methods of administration allows us to tailor treatment in accordance with your specific needs.
- As testified by reviews in constant circulation, a large number of our patients have found considerable alleviation of symptoms.


Success Rate of Stem Cell Therapy for Brain Injuries at Swiss Medica
At Swiss Medica, up to 80% of patients experience noticeable improvements after stem cell therapy. Many share their recovery stories on our YouTube channel, showing positive changes during and after treatment.
Most of the new patients come through referrals, which portray the level of trust and satisfaction of those treated. We do offer the option of meeting with past patients for consultation on the process, benefits involved, and expectations; this can be helpful as a means of getting a third-party perspective prior to starting treatment.
A patient’s Success Story
For others looking for an answer to the question, ‘Can stem cells repair brain damage?’, patient testimonials can give some of the real information regarding the efficacy as well as safety pertaining to the treatment.
At Swiss Medica, patient stories highlight not only the significant improvements from stem cell therapy, but also the exceptional care and support provided throughout their treatment journey. Their reviews reflect both medical benefits and the compassionate experience they received.
Story of Daniel from USA
Daniel was diagnosed 30 years ago with a severe brain stem injury; attending physical therapy did little to improve his condition. Extensive research on various stem cell clinics led him to seek treatment at Swiss Medica.
His treatment program lasted 10 days and encompassed advanced stem cell therapies in an attempt to address his condition. The program included:
- Intrathecal Injection: One injection of autologous bone marrow MNC was directly administered into the spinal canal, targeting the injury within the brain stem.
- Intramuscular Injection: Allogeneic cultivated umbilical cord-derived multipotent mesenchymal stromal cells were injected intramuscularly to assist in the repair and regeneration of tissue.
- Intravenous Infusion: The allogeneic cultivated placenta-derived multipotent mesenchymal stromal cells would be administered through IV for better healing and minimizing inflammation.
This broad approach was supposed to bring regeneration benefits that could hopefully affect Daniel’s condition, which had seen very little progress for decades with conventional therapies.
“What really impressed me about Swiss Medica was that they do a lot of research. They approach the treatment from a professional standpoint, explaining what’s going to work and what’s not. It’s not just an ad campaign—it’s fact-based.”
Does Stem Cell Therapy Cure Brain Injuries?
Although promising, this kind of treatment with stem cells neither promises complete recovery nor a cure of a brain injury. The outcomes may be variable depending on the type and severity of the injury, the individual health of the patient, and how sooner the treatment after the injury begins.
Stem cells may aid brain regeneration and improve motor, sensory, and cognitive functions. They’ve shown potential in treating brain injuries from trauma, stroke, and hypoxic-ischemic attacks. However, outcomes range widely, and current research on stem cell therapy for traumatic brain injury is still evolving.
Brain Injury Stem Cell Treatment Cost
Brain stem cell treatment cost may vary considerably depending on factors such as the type of stem cells used, the kind of clinic or hospital, and the number of sessions.
Key factors affecting the price include:
- Stem cell type
- The number of sessions required
- The location of the facility
- Pre and post-care
In the U.S. and Europe, treatment typically ranges from $20,000 to $50,000. This often excludes travel, accommodation, and rehabilitation costs, so it’s important to inquire thoroughly about all expenses. At Swiss Medica, brain stem cell treatment cost typically ranges from €7,000 to €31,000*, depending on the complexity and number of sessions needed. Transparent pricing and personalized treatment plans are provided after consultation.
*The prices mentioned are indicative and subject to change based on individual factors, including the condition’s severity and the number of stem cells needed. Prices are valid as of January 2025.
Stem Cell Research for Brain Injury
Stem cell research for brain injury is an exciting area in regenerative medicine. It focuses on repairing brain tissue damaged by conditions like TBI and stroke. Mesenchymal stem cells (MSCs) and neural stem cells (NSCs) show promise in generating new neurons, regulating immune responses, and stimulating blood vessel growth. Besides exploring the newest stem cell treatments for traumatic brain injury, researchers work on improved delivery methods, such as injecting stem cells into the brain and intranasal delivery to bypass the blood-brain barrier.
Despite progress, challenges remain, including ensuring long-term safety and avoiding immune rejection. iPSCs, derived from adult cells, offer an ethical alternative to embryonic stem cells. Future research aims to optimize delivery methods like intracerebral injections and explore combining stem cell therapy with rehabilitation or drugs for better recovery.
Clinical Trials of Stem Cell Treatment for Brain Damage
Studies report enhanced quality of life and motor function, especially when stem cells are administered shortly after injury. Large-scale studies confirm long-term outcomes and thereby help promote development into the newest stem cell treatments for traumatic brain injury.
In pediatric TBI cases, stem cell therapy has been observed to lower intracranial pressure and improve neurological functions, suggesting younger patients may experience more significant recovery potential.
Brain Damage Stem Cells: Questions and Answers
1. Can Stem Cells Heal Brain Damage?
Now it is not possible to completely cure brain damage with the help of stem cell therapy. However, it can help repair damaged tissues of the brain, improve brain function, and also decrease symptoms of a number of neurological diseases. The condition of the patient may improve, but that would depend on the severity of the damage, the type of damage in the brain, and how the body of the patient responds to the treatment.
2. What Are the Advantages of the Use of Stem Cells in Treating Brain Injuries?
In general, the aim of stem cell transplants for brain injury is the probable regeneration of neurons, reduction of inflammation, and release of neuroprotective factors to promote the actual healing of brain injuries. They can also induce the formation of new blood vessels (angiogenesis) and create conditions that are favorable for the recovery of brain tissue.
3. How Safe is the Treatment of Brain Injuries with Stem Cells?
Generally speaking, stem cell treatment is safe as long as it is being performed by experienced doctors in good facilities. The procedure has been found to be very safe with very minimal side effects.
4. How Long Does It Take to Notice the Effectiveness of the Stem Cell Treatment in Traumatic Brain Injuries?
Results vary according to each patient and the nature of his/her injury. Some may see an improvement in a few weeks/months, while it takes longer for other patients to observe the desired results. In fact, in the case of most patients, multiple treatments with stem cells are necessary besides follow-ups. Improvement usually progresses gradually, such as in cognition, motor functions, or speech, for example.
5. Does Insurance Pay for The Treatment of Brain Injuries Using Stem Cells?
Most of the time, insurance does not cover it, and patients have to pay out of pocket. It is always advisable that the patients should ask for all the details from their insurance providers because the policies may have variability as regards the brain stem cell treatment costs and, in addition, also the kind of stem cell therapy being provided.
Send a request
Contact us to learn about the expected results of the treatment, its cost and duration.

Medical Advisor, Swiss Medica doctor
List of References
Schepici G, Silvestro S, Bramanti P, Mazzon E. Traumatic Brain Injury and Stem Cells: An Overview of Clinical Trials, the Current Treatments and Future Therapeutic Approaches. Medicina (Kaunas). 2020 Mar 19;56(3):137. doi: 10.3390/medicina56030137. PMID: 32204311; PMCID: PMC7143935.
Ria Kakkad. Drug Target Review. New hydrogel stem cell treatment could repair injured brain tissue https://www.drugtargetreview.com/news/108577/new-hydrogel-stem-cell-treatment-could-repair-injured-brain-tissue/
Aderinto, N., Olatunji, G., Kokori, E. et al. Stem cell therapies in stroke rehabilitation: a narrative review of current strategies and future prospects. Egypt J Neurol Psychiatry Neurosurg 60, 79 (2024). https://doi.org/10.1186/s41983-024-00851-7
Zhang S, Lachance BB, Moiz B, Jia X. Optimizing Stem Cell Therapy after Ischemic Brain Injury. J Stroke. 2020 Sep;22(3):286-305. doi: 10.5853/jos.2019.03048. Epub 2020 Sep 29. PMID: 33053945; PMCID: PMC7568970.
Harting MT, Baumgartner JE, Worth LL, Ewing-Cobbs L, Gee AP, Day MC, Cox CS Jr. Cell therapies for traumatic brain injury. Neurosurg Focus. 2008;24(3-4):E18. doi: 10.3171/FOC/2008/24/3-4/E17. PMID: 18341394; PMCID: PMC3721356.
Xiong Y, Mahmood A, Chopp M. Emerging potential of exosomes for treatment of traumatic brain injury. Neural Regen Res. 2017 Jan;12(1):19-22. doi: 10.4103/1673-5374.198966. PMID: 28250732; PMCID: PMC5319225.
Katz, D. I., & Alexander, M. P. (2022). Neuroimaging and biomarkers in traumatic brain injury: A review. Neurology, 99(1), e1-e12. https://doi.org/10.1212/WNL.0000000000011450
Adugna DG, Aragie H, Kibret AA, Belay DG. Therapeutic Application of Stem Cells in the Repair of Traumatic Brain Injury. Stem Cells Cloning. 2022 Jul 13;15:53-61. doi: 10.2147/SCCAA.S369577. PMID: 35859889; PMCID: PMC9289752.
Lin WY, Wu KH, Chen CY, Guo BC, Chang YJ, Lee TA, Lin MJ, Wu HP. Stem Cell Therapy in Children with Traumatic Brain Injury. Int J Mol Sci. 2023 Sep 28;24(19):14706. doi: 10.3390/ijms241914706. PMID: 37834152; PMCID: PMC10573043.
Zhou, Y., Shao, A., Xu, W., Wu, H., & Deng, Y. (2019). Advance of stem cell treatment for traumatic brain injury. Frontiers in Cellular Neuroscience, 13, 301. https://doi.org/10.3389/fncel.2019.00301
Narouiepour, A., Ebrahimzadeh-bideskan, A., Rajabzadeh, G. et al. Neural stem cell therapy in conjunction with curcumin loaded in niosomal nanoparticles enhanced recovery from traumatic brain injury. Sci Rep 12, 3572 (2022). https://doi.org/10.1038/s41598-022-07367-1
MD, Pediatrician, Regenerative Medicine Specialist







