For people with advanced pulmonary fibrosis, even simple tasks like walking can become extremely difficult. The persistent cough and shortness of breath that come with the disease severely affect their quality of life. Current treatments often just slow down the progression and leave many patients searching for better options.
That’s where stem cell therapy for pulmonary fibrosis steps in and offers potential hope. Stem cells, with their ability to regenerate damaged tissues, could be the breakthrough needed for treating lung diseases.
So, can stem cells cure lung fibrosis? Or at least, can stem cell therapy help pulmonary fibrosis in some way? Let’s take a look at what’s currently known.
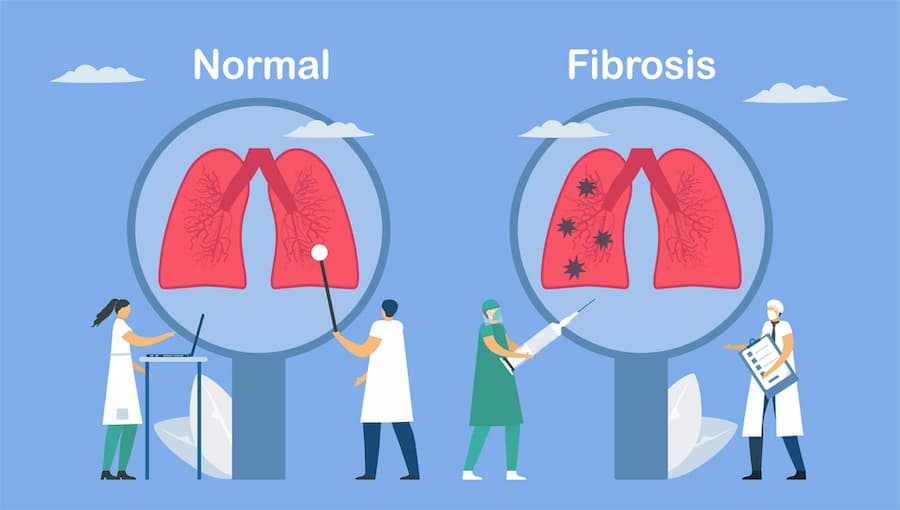
What Is Pulmonary Fibrosis, and How Does It Affect the Lungs?
Pulmonary fibrosis is a serious condition that affects the lungs, characterized by a thickening and scarring of lung tissue. This affects the lungs right down to the alveoli, where oxygen is exchanged.
There are several factors that can contribute to this lung damage. For instance, long-term exposure to harmful substances, radiation treatments, certain medications, and various health issues can all play a role. In some cases, doctors aren’t able to pinpoint a specific cause.
As the condition worsens over time, the lung tissue becomes stiff and hard, which makes it more difficult to breathe. Many people with pulmonary fibrosis find that they struggle with shortness of breath during activities that used to be easy, like climbing stairs or even walking around the house.
How Stem Cell Therapy Works for Pulmonary Fibrosis
Lung fibrosis stem cell treatment uses the potential of stem cells to support the repair of damaged lung tissue. The treatment involves injecting stem cells, usually taken from bone marrow or fat, into the lungs or through an IV infusion. Once these cells reach the lungs, they can promote tissue regeneration.
Stem cells also release signaling molecules that help modulate the inflammatory environment in the lungs. This can reduce inflammation and contribute to the remodeling of the lung tissue.
Benefits of Stem Cell Therapy for Pulmonary Fibrosis Patients
Stem cell therapy for lung fibrosis offers many benefits that can enhance the quality of life for patients facing this disease:
Improved respiratory function
One major benefit of using stem cells for pulmonary fibrosis is better lung function. A recent study found that patients treated with mesenchymal stem cells for lung fibrosis showed an improvement in forced vital capacity—a key measure of lung performance—over 52 weeks. The MSC group improved significantly, while the placebo group barely changed.
Are you curious about which stem cells are used in therapy and how they differ?
Find out in our article.
Slowing down the progression of fibrosis
Stem cell therapy can also slow the progression of pulmonary fibrosis. A recent analysis of 24 studies showed that patients receiving MSC treatment had a higher survival rate compared to those who did not receive stem cells.
Minimal side effects compared to other treatments
Unlike many traditional treatments, therapy involving stem cells for pulmonary fibrosis has fewer side effects. Research indicates that MSCs can support the repair of injured lung tissue without causing serious complications.
Stem Cell Therapy vs. Traditional Pulmonary Fibrosis Treatments
The table below compares traditional and stem cell therapies.
| Stem cell therapy | Traditional treatments | |
| Mechanism of action | Promotes repair and regeneration of lung tissue | Alleviates symptoms, slows disease progression |
| Treatment type | Innovative, emerging therapy | Established, standard care |
| Efficacy | Potential for improved lung function and quality of life | Varies by individual, often less effective over time |
| Side effects | Minimal side effects | Common side effects include nausea, diarrhea, etc. |
| Long-term outcomes | Still under research | Limited long-term benefits; disease often progresses |
| Patient selection | May be suitable for certain patients with severe cases | Widely available, used for all stages of PF |
To enhance the therapeutic effect, some researchers propose combining stem cell treatment for pulmonary fibrosis with medication for better results.
Risks and Side Effects of Stem Cell Therapy for Pulmonary Fibrosis
Treatment with mesenchymal stem cells in pulmonary fibrosis is generally safe, but there are some risks to consider.
In most cases, clinical studies show that MSCs have only minor side effects. For instance, about 22% of patients receiving human umbilical cord MSCs for COVID-19 treatment experienced mild fever, which is manageable.
Other side effects may include:
- Fatigue,
- Headaches,
- Nausea,
- Chills,
- Pain or discomfort at the injection site.
We’re here to help you understand the safety and potential side effects of stem cell therapy. Our goal is to ensure you’re fully informed so you can make the best decision for your health.
Read more about safetyWho Can Benefit From Stem Cell Therapy for Pulmonary Fibrosis?
Using stem cells for pulmonary fibrosis may benefit several specific groups of patients:
| Patients with idiopathic pulmonary fibrosis | Those diagnosed with IPF, a type of fibrosis with no known cause, often have limited treatment options. Stem cell therapy can offer potential improvement in lung function and slow disease progression. |
| Patients unresponsive to medications | Individuals who haven’t seen positive results from traditional treatments like corticosteroids or antifibrotic drugs may turn to stem cell therapy as an alternative for symptom relief. |
| Early-stage pulmonary fibrosis patients | Those in the earlier stages of the disease may benefit from stem cell therapy to slow the progression of fibrosis and preserve lung function longer. |
| Patients seeking minimally invasive options | Modern medicine offers insufficient pharmacological treatments. In addition, lung transplantation remains the only possible treatment for patients suffering from end-stage PF. But the complexity of the transplant surgery and the shortage of donors significantly limit this method of treatment. Due to their pluripotency and paracrine effects (where cells release signaling molecules), stem cells are a promising therapy for interstitial lung diseases. |
| Older adults or high-risk patients | Stem cell therapy may be a good fit for older patients or those with other health conditions that make them unsuitable candidates for surgeries or aggressive treatments. |
Contact us
Think you might be a candidate? Let our specialists help you find out. Fill out the form for a free online consultation, and our experts will assess how stem cell therapy could support your lung health.

Medical Advisor, Swiss Medica doctor
How to Find the Best Stem Cell Clinic for Stem Cell Therapy for Lung Fibrosis?
Choosing the right clinic for stem cell therapy is an important step in treating lung fibrosis. It’s essential to consider expertise, treatment options, and patient support.
At Swiss Medica, we provide comprehensive care, starting with a no-obligation online consultation with our regenerative medicine experts. During this consultation, we’ll explain how stem cell therapy can benefit you, discuss treatment costs and timelines, and develop a personalized treatment plan tailored to your needs.
Once you decide to move forward, we ensure you’re well-supported throughout the process. This begins with the evaluation of lab tests and imaging to fully assess your condition. In addition to stem cell therapy, we offer complementary treatments such as recovery therapies and physiotherapy to enhance your healing. We also help with travel arrangements, accommodation, and meals tailored to your preferences.
After your treatment, our medical team is always available to answer your questions and provide daily check-ins from various specialists.
Why Choose Swiss Medica for Stem Cell Treatment for Pulmonary Fibrosis?
If you’re considering stem cell treatment, here’s what Swiss Medica has to offer:
Expert team
Our dedicated team of stem cell specialists brings over 12 years of experience, ensuring expert, high-quality care.

Personalized approach
Our doctors take the time to thoroughly understand your symptoms and medical history before creating a personalized treatment plan tailored to your needs. We also offer follow-up programs to ensure long-lasting results and continued support.
Comfortable atmosphere
Our clinic and hospital are designed to feel like a hotel rather than a typical hospital. We focus on your comfort, providing meals that meet your dietary needs and preferences. Plus, our staff is available around the clock to assist you whenever you need help.
Commitment to quality
Our in-house laboratory follows strict safety and ethical guidelines to produce high-quality stem cell products. We monitor every dose to make sure it’s safe and effective.
Success Rate of Stem Cell Therapy for Lung Fibrosis at Swiss Medica
Since we started operating in 2011, Swiss Medica has supported over 10,000 patients in improving their quality of life with stem cell therapy. About 80% of them have reported positive results. This success is a testament to the hard work and dedication of our team of stem cell specialists and medical professionals.
Learn more about our patients’ experiences and their results.
Check out our patient’s testimonialsCost of Stem Cell Therapy for Pulmonary Fibrosis Treatment
Swiss Medica was founded in Switzerland in 2011 and, since 2016, our main therapeutic clinic has been located in Belgrade, Serbia. The country offers a supportive medical environment, experienced doctors, and convenient access for international patients — ensuring high-quality treatment in a welcoming setting.
In fact, the cost of using stem cells for pulmonary fibrosis in Serbia is generally lower than in countries like the USA and UK. Patients typically spend between €7,000 and €31,000* for their treatment.
*The prices mentioned are indicative and subject to change based on individual factors, including the condition’s severity and the number of stem cells needed. Prices are valid as of January 2025.
Stem Cell Success With Pulmonary Fibrosis: Real Patients
There are a number of reports detailing stem cell success with pulmonary fibrosis.
Case 1. This report described a critically ill COVID-19 patient with pulmonary fibrosis who showed significant improvements after receiving two doses of umbilical cord-derived MSCs. Following the treatment, the patient’s oxygen levels improved, inflammation reduced, and lung scans showed better results. There were no serious side effects from the therapy.
Case 2. Another case involved a 56-year-old man with COPD and IPF. After receiving stem cell therapy, his lung function and CT scores improved over 12 months, with a noticeable decrease in fibrosis.
Stem Cell Research on Pulmonary Fibrosis
Stem cell research on pulmonary fibrosis is looking into their potential to treat lung damage, and results indicate their ability to target damaged lung tissue.
For example, in 2013, results were published from the first international clinical trial on cell therapy for ILF, conducted in Greece. Patients with mild to moderate lung function impairment received three monthly infusions of their own adipose (fat) tissue stem cells, with each dose based on body weight. The 12-month follow-up showed no serious side effects, and lung function remained stable in terms of forced vital capacity, carbon monoxide diffusion capacity, and a 6-minute walk test.
A bibliometric analysis from 2002 to 2021 shows the therapeutic potential of MSCs in pulmonary fibrosis. MSCs help reduce inflammation and promote tissue repair by releasing anti-inflammatory and antifibrotic factors.
Stem Cell Therapy for Lung Fibrosis: Clinical Trials
Stem cell therapy for pulmonary fibrosis is currently being researched, with clinical trials underway to explore its effectiveness, safety, and how well patients tolerate it. Studies have shown promising results, and the field is progressing with the potential for future breakthroughs.
These studies explore several critical factors:
- One is finding the best delivery method to get stem cells to the lungs, where they can help repair damaged tissue.
- Another important question is how to encourage stem cells to differentiate into lung epithelial cells, which is essential for them to have a lasting therapeutic effect.
Researchers are also investigating the optimal dosage and timing for administering stem cells to achieve the best outcomes.
FAQ: Stem Cell Therapy for Pulmonary Fibrosis
1. Can stem cells help pulmonary fibrosis?
Stem cells show promise in treating pulmonary fibrosis by reducing inflammation and promoting tissue repair. Their regenerative properties may help slow the progression of the disease, protect lung tissue from further damage, and improve overall lung function.
2. Is stem cell therapy a permanent solution?
The results of stem cell therapy can vary depending on the individual. For some patients, it may provide long-term benefits, but there is no guarantee of permanence. In many cases, follow-up treatments may be necessary to maintain or enhance the effects.
3. Where can I find stem cell therapy for pulmonary fibrosis?
Swiss Medica offers stem cell treatment for pulmonary fibrosis, with personalized treatments and expert care. Our team of medical experts works closely with you to ensure comprehensive care, using the latest regenerative medicine techniques. Along with stem cell therapy, we offer additional treatments such as physiotherapy and recovery programs to support your healing and improve long-term outcomes.
Get a free online consultation
Pulmonary fibrosis can feel like a constant battle, but stem cell therapy might help you regain control. Complete the form to schedule a free online consultation with one of our experts and explore how this treatment could improve your symptoms and overall well-being.

Medical Advisor, Swiss Medica doctor
List of References:
Ikrama M, Usama M, Israr S, Humayon M. Pulmonary fibrosis: Is stem cell therapy the way forward? J Taibah Univ Med Sci. 2023 Oct 11;19(1):82-89. doi: 10.1016/j.jtumed.2023.09.009. PMID: 37876594; PMCID: PMC10590845.
Muhammad Ikrama, Muhammad Usama, Shifa Israr, Maryam Humayon,Pulmonary fibrosis: Is stem cell therapy the way forward?,Journal of Taibah University Medical Sciences,2024,ISSN 1658-3612, https://doi.org/10.1016/j.jtumed.2023.09.009.(https://www.sciencedirect.com/science/article/pii/S165836122300149X)
Cheng, W., Zeng, Y. & Wang, D. Stem cell-based therapy for pulmonary fibrosis. Stem Cell Res Ther 13, 492 (2022). https://doi.org/10.1186/s13287-022-03181-8
William T. Schmidt, Gregory P. Cosgrove, Pauline Bianchi, RN Harold Collard, MD Kevin R. Flaherty, MD, MS. AN UPDATE OF STEM CELL/CELL-BASED THERAPIES FOR PULMONARY FIBROSIS BEYOND THE CONTEXT OF CLINICAL TRIALS A word of caution by the Medical Advisory Board of the Pulmonary Fibrosis Foundation (PFF) March 5, 2019 https://www.pulmonaryfibrosis.org/researchers-healthcare-providers/clinical-resources/position-statements/stem-cell-cell-based-therapies-for-pulmonary-fibrosis
American Lung Association. Statement on Unproven Stem Cell Interventions for Lung Diseases https://www.lung.org/lung-health-diseases/wellness/public-health-issues-lung-health/stem-cell-therapy
Qi Lu and Ahmed H. K. El-Hashash. Cell-based therapy for idiopathic pulmonary fibrosis. Stem Cell Investigation, 2019. https://sci.amegroups.org/article/view/28199
Nakamura, Y.; Niho, S.; Shimizu, Y. Cell-Based Therapy for Fibrosing Interstitial Lung Diseases, Current Status, and Potential Applications of iPSC-Derived Cells. Cells 2024, 13, 893. https://doi.org/10.3390/cells13110893
Yang Shengnan , Liu Peipei , Jiang Yale , Wang Zai , Dai Huaping , Wang Chen. Therapeutic Applications of Mesenchymal Stem Cells in Idiopathic Pulmonary Fibrosis. Frontiers in Cell and Developmental Biology. 2021 https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.639657
MD, Pediatrician, Regenerative Medicine Specialist







