What are macrophages?
Monocyte/Macrophage originate in the bone marrow and enter the peripheral blood. During inflammation, circulating monocytes leave the blood flow and migrate into tissues. They differentiate into macrophage following exposure to local growth factors, proinflammatory cytokines, and microbial products.
Macrophages have multiple functions:
- Phagocytosis of pathogens, infected, debris, and dead cells
- Antigen presentation
- Production of different type of cytokines, (interleukin-1 (IL-1), IL-6, tumor necrosis factor-α (TNF-α) and etc.
In addition, macrophages play important roles in the progression of inflammatory diseases, including diabetes, cancer, atherosclerosis and diseases of the central nervous system (CNS).
Studies over the last two decades have demonstrated that macrophages could cause both neurodestructive and neuroreparative effects. This dual impact is related to the heterogeneity of macrophages [1].
What are M2 macrophages?
Macrophages within CNS comprise microglia and CNS-infiltrating macrophages.
Actually, there are at least two functional macrophage subpopulations: “classical” proinflammatory (M1) and anti-inflammatory (M2) macrophages.
Intensive acute danger signal or it’s chronic activation directs microglia towards M1 neurotoxic phenotype, while short-term or moderate signal induces M2 regenerative phenotype.
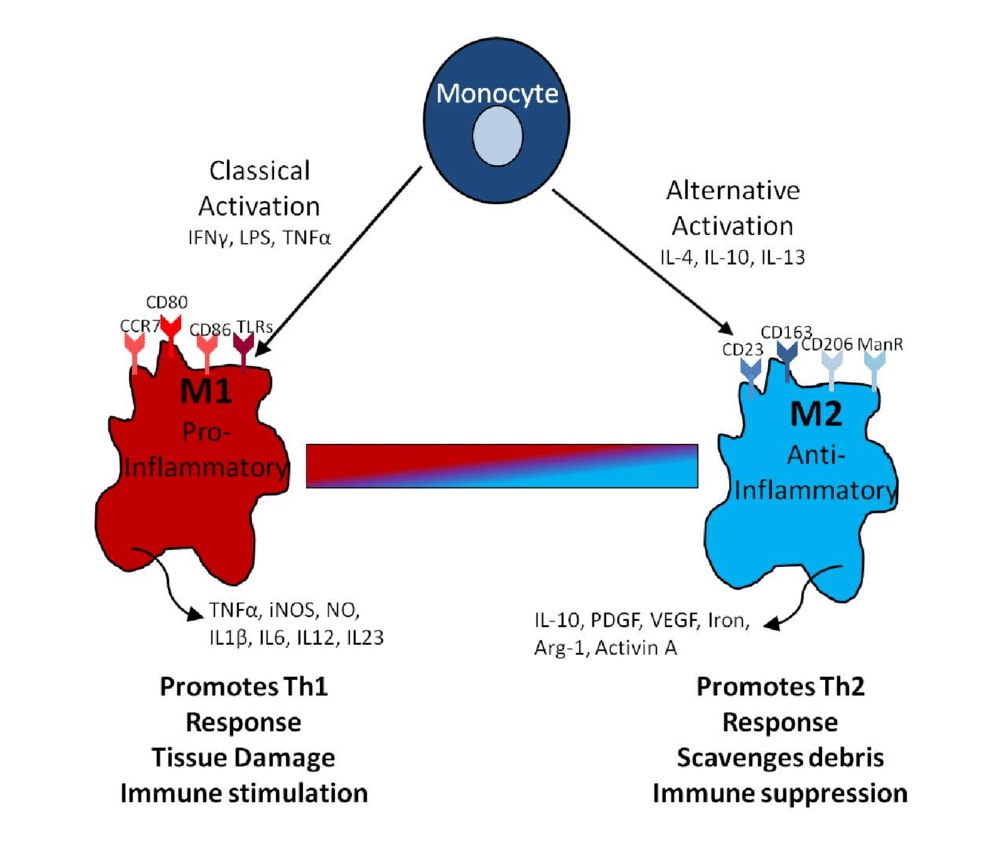
Two functional macrophage subpopulations
M1 cells support inflammation, mediate resistance to intracellular pathogens and tumor resistance, but are tissue destructive. In contrast, M2 cells display anti-inflammatory and immunoregulatory activity, stimulate angiogenesis, and activate tissue repair [2]. In addition, M2 macrophages induce predominantly T helper 2 cell (Th2) response that is particularly beneficial in the repair of the CNS.
Properties of М2-type alternatively activated macrophages:
- anti-inflammatory activity
- mediate neuroprotection
- activate neuro- and angio-genesis
- play an essential role in neuronal plasticity
- participate in axon remodelling
In accordance with this notion, therapeutic approaches targeting macrophage polarisation towards M2 phenotype has been considered as a novel strategy for stimulating neuroreparative processes [3].
How safe is the use of M2 macrophages?
Pilot study of M2 intrathecal administrations in 30 adults with ischemic stroke [4] demonstrated the safety and improvement of motor and cognitive functions. No serious adverse events were observed.
Another study of 21 child with cerebral palsy [5] showed no adverse events. No cases of mortality, psychomotor worsening, exacerbation of seizures, and long-term comorbidities, including tumors, were observed during a 5-year follow-up.
However, there are 2 main serious challenges for this treatment. First of all, the invasiveness of intrathecal injection creates risks of side effects from injection. Secondly, there is a possibility of M2→M1 repolarization in the pathological environment of the patient’s brain tissue.
Get a free online consultation
Please, contact our medical advisor to discuss your health condition with a specialist in regenerative medicine. You can also leave your contact details for a callback. It is free and confidential.
MD, Endocrinologist, Pediatrician, regenerative medicine specialist, R&D director
What are the alternatives?
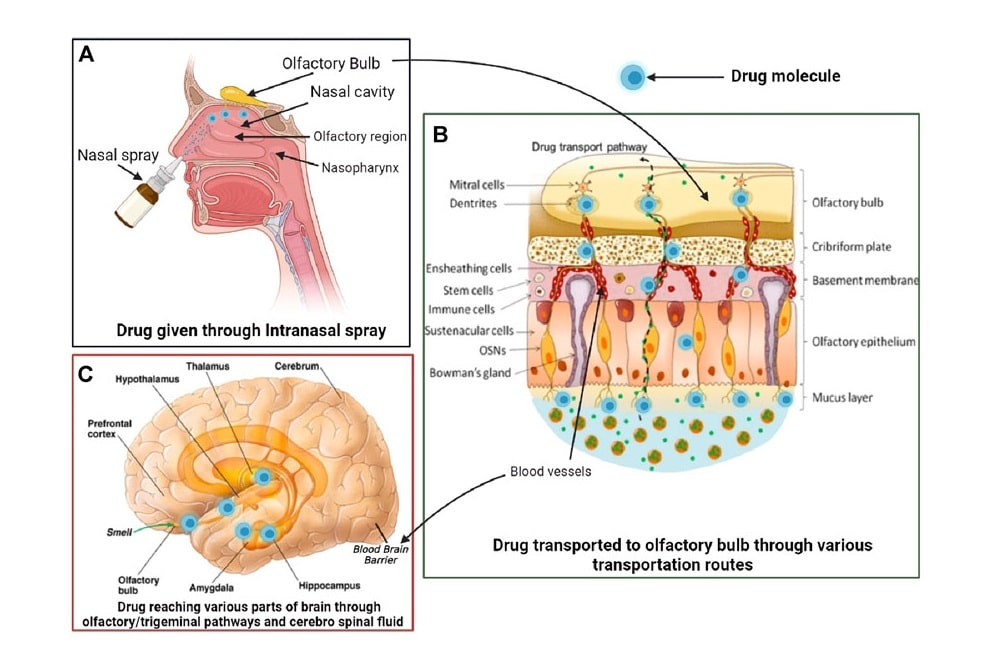
In this connection, the utilization of M2-derived soluble products (secretome/exosomes) instead of cells and intranasal administration appears to be a promising approach.
Exosomes guarantee the safety of treatment, since it is not the M2 cells that are transported (which can repolarize into M1 macrophages and increase inflammation), but only their products.
Intranasal administration allows a rapid delivery of substances (including neurotrophic factors) to the brain via olfactorial and trigeminal route bypassing blood-brain barrier.
The utilization of M2-derived soluble products (secretome/exosomes)
A possibility for cytokines and hormones to be delivered into brain tissue upon intranasal route of delivery has been demonstrated in experimental models as well as in humans [6][7].
Also, the feasibility of intravenous administration of M2 macrophages is discussed. Given the ability of macrophages to independently move to the area of inflammation, this approach may have a systemic anti-inflammatory effect.
How is M2 macrophage therapy performed?
We use the patient’s own cells or those of a relative for treatment. Before starting treatment, we collect a blood sample and isolate monocytes from it. Further, in the laboratory, polarization is carried out towards M2 Macrophages and the collection of secreted factors (Secretom / Exosomes). This process will take about 8-9 days.
The cells can then be administered intravenously to the patient, and the Exosomes are administered via nasal drops and issued to the patient to continue treatment after discharge from the clinic.
As a rule, macrophage therapy is carried out in combination with other regenerative methods, such as mesenchymal stromal cells and their derivatives.
What effects can be expected after treatment?
The study of using M2-derived soluble products in 30 patients with chronic cerebrovascular disease was found to be safe and well tolerated [8]. Neuropsychological improvements showed the amelioration of neurological symptoms, reduction in anxiety and depression levels, improvement in balance and gait ability as well as cognitive functions. Clinical effects could be detected in 30 days and were stable during 6-month follow-up.
Functional brain restoration is achieved by means of activation of such processes, as neuroplasticity, neurogenesis and angiogenesis. They are controlled by an array of neurotrophic (NGF, BDNF, GDNF, and NT 4/5) and growth (IGF-1, FGF-basic, EGF, EPO, and VEGF) factors [9].
The M2 secretome profile is quite similar to that characteristic of mesenchymal stem cells (MSCs). This observation laid the foundation for using M2 macrophage secretome products with a view to treat patients with other neurological conditions, including autism spectrum disorder.
Contact us
Get a free online consultation to learn about the expected results of stem cell therapy for your case, what is the cost of the treatment, and its duration.
MD, Endocrinologist, Pediatrician, regenerative medicine specialist, R&D director
References
List of References:
Gordon S, Taylor PR. Monocyte and macrophage heterogeneity. Nat Rev Immunol. 2005, 5(12): 953–964.
Mantovani, A.; Biswas, S. K.; Galdiero, M. R.; Sica, A.; Locati, M. Macrophage plasticity and polarization in tissue repair and remodelling. J. Pathol. 229:176–185; 2013.
Hu XM, Li PY, Guo YL, et al. Microglia/macrophage polarization dynamics reveal novel mechanism of injury expansion after focal cerebral ischemia. Stroke. 2012, 43(11): 3063–3070.
Chernykh ER, Shevela EY, Starostina NM, et al. Safety and therapeutic potential of M2-macrophages in stroke treatment. Cell Transplant. 2016, 25(8): 1461–1471.
Chernykh ER, Shevela EY, Kafanova MY, et al. Monocytederived macrophages for treatment of cerebral palsy: A study of 57 cases. J Neurorestoratology. 2018, 6: 41–47.
Alcalá-Barraza SR, Lee MS, Hanson LR, et al. Intranasal delivery of neurotrophic factors BDNF, CNTF, EPO and NT-4 to the CNS. J Drug Target. 2010, 18(3): 179–190.
Dhuria SV, Hanson LR, Frey WH. Intranasal delivery to the central nervous system: mechanisms and experimental considerations. J Pharm Sci. 2010, 99(4): 1654–1673.
Chernykh ER, Shevela EY, Starostina NM, et al. Intranasal delivery of M2 macrophage-derived soluble products reduces neuropsychological deficit in patients with cerebrovascular disease: a pilot study. Journal of Neurorestoratology. 2019, 7(2): 89–100.
Yang XT, Bi YY, Feng DF. From the vascular microenvironment to neurogenesis. Brain Res Bull. 2011, 84(1): 1–7.
MD, Endocrinologist, Pediatrician, regenerative medicine specialist, R&D director







