Mesenchymal stromal cells (MSCs), also known as multipotent stromal cells, are a type of cell found in a variety of tissues, including bone marrow, fat, gums, peripheral blood, as well as the placenta and umbilical cord. They are commonly referred to as “stromal” because they reside in the supportive network of tissues, providing structure and support to other cells. However, their role extends beyond mere support.
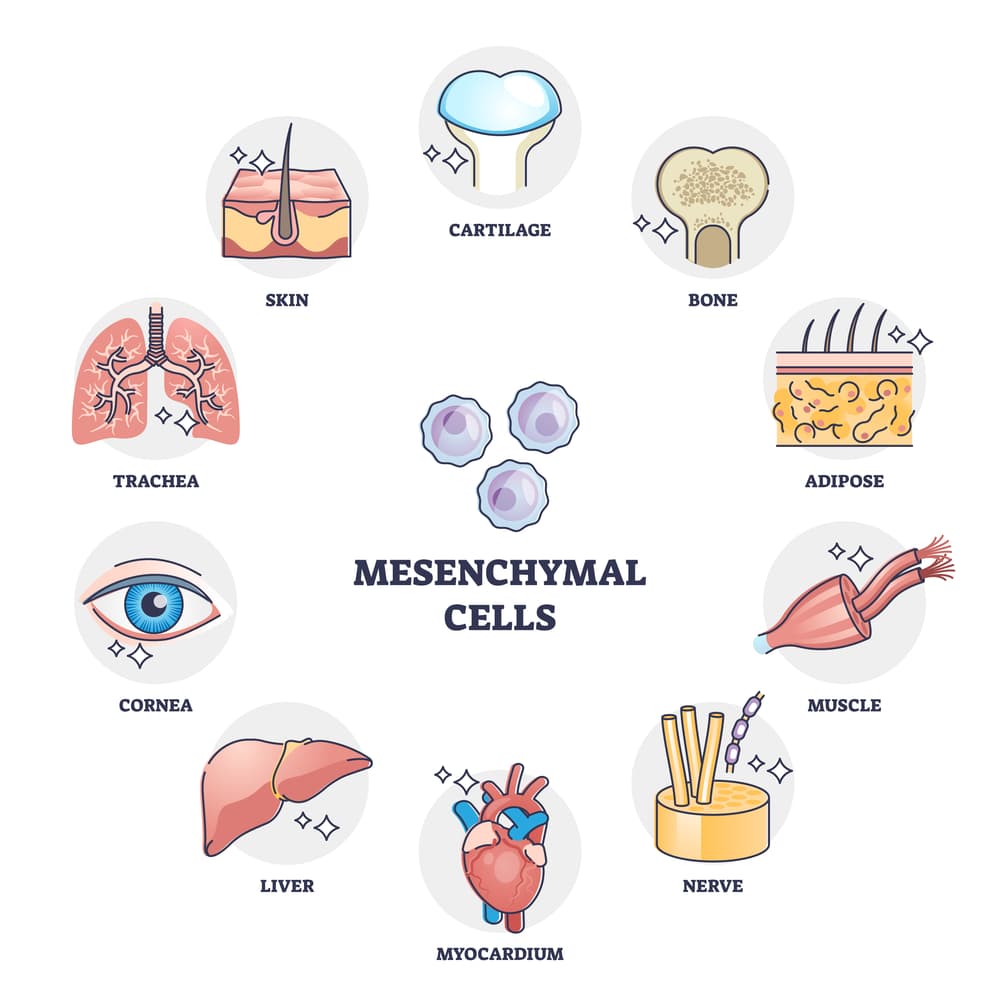
Research indicates that MSCs can differentiate into a wide range of cell types, including bone, cartilage, fat, neural, and muscle cells. This makes them a promising candidate for regenerative medicine, with the potential to treat a variety of diseases and injuries.
Get a free online consultation
Every condition is unique. How does mesenchymal stem cell therapy work for your specific case? Schedule a no-obligation online consultation with our medical advisors. They’ll provide personalized guidance and answer any questions you may have.

Medical Advisor, Swiss Medica doctor
What Makes MSCs So Special: Main Functions for Therapy
MSCs can support other cells and enhance the body’s immune system through their main functions:
| Main Function | How Do Mesenchymal Stem Cells Work? |
| Paracrine regulation | MSCs have the unique ability to activate the patient’s own stem cell pool and regenerative capacity. They secrete a diverse set of bioactive molecules, such as growth factors, cytokines, and extracellular vesicles. These molecules can influence the surrounding microenvironment, promoting tissue repair and decreasing inflammation. |
| Immunomodulatory properties | MSCs can suppress immune responses, making them useful for controlling autoimmune conditions. |
Concerned about the safety of stem cells?
Check out our article on safety and adverse effects to learn more.
When Do We Use MSCs
MSCs have a very broad range of applications. It includes all chronic diseases accompanied by massive cell death and damage, such as autoimmune and degenerative diseases.
How do mesenchymal stem cells work in each specific case?
| Bone regeneration | Cartilage repair | Blood vessel engineering | Autoimmune diseases |
| MSCs can stimulate the differentiation of osteoblasts—the cells responsible for bone formation—potentially treating bone fractures and osteoporosis. | MSCs can stimulate cartilage cell generation, offering hope for treating osteoarthritis and other cartilage-related conditions. | MSCs can stimulate the growth of new blood vessels, which is important for degenerative diseases like multiple system atrophy and cerebral small vessel disease. | MSCs can modulate the immune system and improve neuromuscular conduction, potentially slowing the progression of conditions like multiple sclerosis, lupus, and rheumatoid arthritis. |
MCSs are also effective for recovery from injuries, surgeries, acute heart attacks, and strokes.
Mesenchymal Stromal Cell Collection and Preparation
Mesenchymal stem cells fall into two main categories:
- donor cells
- autologous cells.
At Swiss Medica, we use both types of MSCs.
Want to understand the difference between donor and autologous stem cells? Discover the details in our article.
Read moreHow does mesenchymal stem cell therapy work, depending on the type used?
Donor Cells
We only use donor cells from tissues that the mother voluntarily donated after a healthy childbirth. Before taking a cell sample, we have access to all test results and the pregnant woman’s medical history. Our stem cells may come from:
- Placental tissue—a temporary organ that forms in the uterus during pregnancy and connects the baby to it.
- Umbilical cord tissue that connects the fetus and the placenta.
The cells can be collected at the time of birth and stored for later use.
We thoroughly examine each stem cell product multiple times before using it in a patient’s treatment. With our in-house laboratory, we can closely monitor stem cells’ composition and viability, guaranteeing safe and effective doses.

Explore how our rigorous testing and monitoring processes ensure that each stem cell product meets the highest safety standards before it’s used in treatment.
Keep readingPatient’s Own Cells
We obtain autologous, or the patient’s own cells, from:
- red bone marrow—the soft, porous tissue with numerous blood vessels located at the core of most bones,
- adipose tissue (SVF), also known as body fat,
- gingiva,
- and some other sources.
The patient’s cells can be partially used immediately and partially frozen until the patient’s next visit. Prior to the next arrival, the patient’s cells are cultured in a sterile laboratory environment for 4 to 5 weeks.
We recommend having an additional two months available in case the process takes longer, particularly for older patients whose cells may take longer to grow.
How Do We Deliver the MSCs?
How does mesenchymal stem cell therapy work after cultivation and preparation? The effectiveness of the therapy is closely tied to the delivery method.
We offer donor cells through various methods, including:
- Intravenously. Intravenous administration involves injecting the cells directly into a vein, which allows them to circulate throughout the body via the bloodstream.
- Locally. We can deliver cells directly to a specific area, such as muscles or joints, or through masks, drops, enemas, or inhalations.

Patients may be concerned about the risks of injecting donor cells into specific body cavities, such as the spinal cord or joints. To predict any cell rejections, we thoroughly investigate the patient’s personal history, condition specifics, donor suitability, and so on. This is one of the reasons behind Swiss Medica’s 80% success rate.
With the patient’s cells, we use the most suitable method for the specific treatment.
Explore the various delivery methods for stem cell therapy on our comprehensive page.
Read moreProgram Duration
The duration of the procedure is determined by the specific disease or the patient’s overall health. The program’s minimum duration could be:
- 3 days for programs with the use of donor cells.
- 5 days for programs using autologous, or own, cells from red bone marrow or stromal vascular fraction.
Interested in how our therapies are designed? Check out our detailed guide to understand the treatment process.
Read moreWe only administer injections after receiving detailed test results to ensure there are no contraindications or risks. This means that we are unable to perform them on the first or last day of the program. Furthermore, these treatments and some supportive therapy, such as plasmapheresis procedures, cannot be carried out on the same day.
Want to learn how we enhance stem cell therapy results and how mesenchymal stem cells work in combination with other methods? Discover the innovative methods we use to boost the effectiveness of our treatments.
Read moreDosages
We take great care in measuring the exact number of stem cells needed for every individual case to achieve more consistent results.
For intravenous (IV) infusions in adults, we recommend a dose of 1 to 2 million cells for every kilogram of body weight.
In children, the dose can be higher, up to 3 million cells per kilogram.
For local administration, the doses we use range from 20 to 100 million cells, depending on the volume of liquid that can be injected safely.
Expected Time for Treatment Results
When thinking about ‘How does mesenchymal stem cell therapy work?’, one may wonder when the first results are coming. The effects of the treatment vary from person to person. For most conditions, a patient feels the maximum benefits within 1 to 3 months after starting the treatment.
The positive effects last up to 6–12 months. In some cases, we see a positive effect up to several years.
Eager to start your own treatment journey?
Find out more about the application process at Swiss Medica and how you can take the first step towards better health.
Contraindications
In certain conditions or situations, we either do not proceed with the treatment or use it with caution:
- Patients with a history of cancer (recurrence or remission of less than 5 years) should avoid the treatment.
- Children under the age of 4 and weighing less than 14 kg should not receive intravenous (IV) infusions of the treatment because the use of cell therapy in such young children has not been sufficiently studied.
- Patients with blood coagulation disorders also have limitations on some treatments.
Side Effects
When considering how mesenchymal stem cells work and their potential benefits, it’s also important to be aware of any possible adverse effects. These are possible undesirable reactions that sometimes occur after receiving the treatment:
- Short-term fever,
- Headaches,
- Malaise,
- Aches and pains in muscles,
- Nausea.
Most of these symptoms last only a few hours after the infusion. They may be relieved with painkillers or rest following the procedure.
Contact us
If you’re weighing the pros and cons of MSC therapy for your condition, schedule a no-obligation online consultation with our medical advisors. They can provide personalized advice and help address any concerns you may have.

Medical Advisor, Swiss Medica doctor
Ready to Explore More?
Discover the full potential of stem cells and dive into additional articles.
List of References
Ullah I, Subbarao RB, Rho GJ. Human mesenchymal stem cells – current trends and future prospective. Biosci Rep. 2015 Apr 28;35(2):e00191. doi.org/10.1042/BSR20150025
Wang H, Yao W, Wang Y, Dong H, Dong T, Zhou W, Cui L, Zhao L, Zhang Y, Shi L, Jiang Y. Meta-analysis on last ten years of clinical injection of bone marrow-derived and umbilical cord MSC to reverse cirrhosis or rescue patients with acute-on-chronic liver failure. Stem Cell Res Ther. 2023 Sep 23;14(1):267. doi.org/10.1186/s13287-023-03494-2