Cirrhosis is often called “liver scarring,” but it does not fully describe the real impact on daily life. Many patients deal with ongoing fatigue, swelling, poor appetite, brain fog, and a constant worry about complications. Standard hepatology care is essential—it can slow progression and prevent emergencies. However, it does not always restore liver function once fibrosis is advanced.
That’s why patients start looking for options that may help them regain stability and improve daily quality of life. At Swiss Medica, stem cell therapy for cirrhosis is delivered as part of a structured medical program for suitable candidates, focused on supporting liver function and reducing the burden of symptoms.
This article explains cirrhosis in simple terms, summarizes what evidence suggests, clarifies who may benefit, and shows how to evaluate a clinic responsibly.
What Is Liver Cirrhosis and Why Does It Progress?
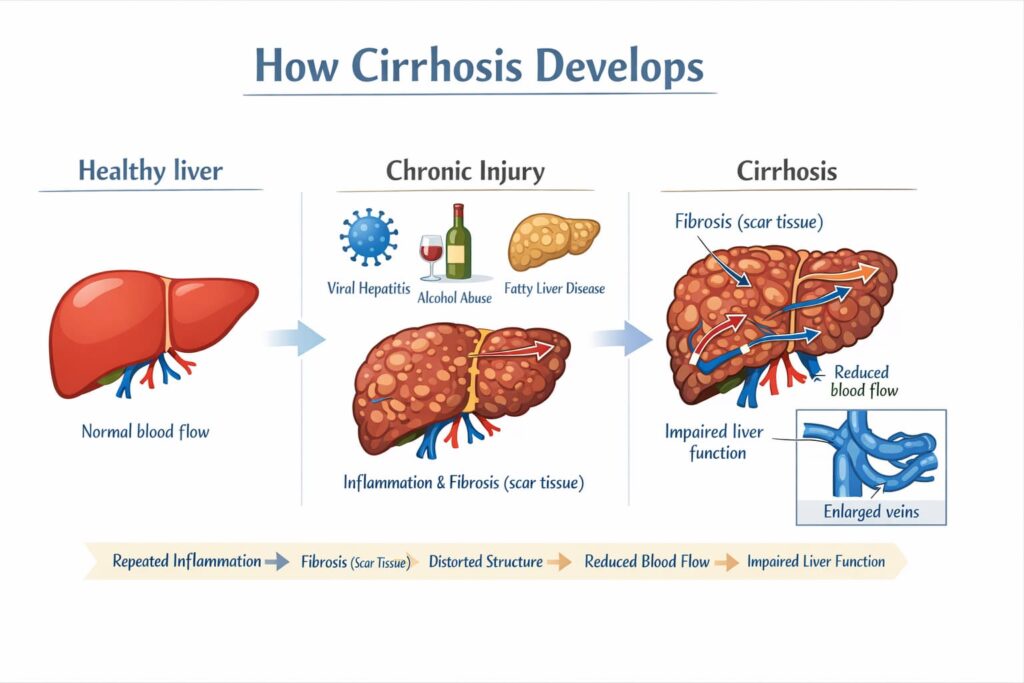
Cirrhosis develops after years of ongoing liver injury caused by conditions such as chronic alcohol use, viral hepatitis, metabolic fatty liver disease, or autoimmune disorders.
Over time, repeated inflammation leads to fibrosis, which changes the structure of the liver. Blood flow becomes harder, and healthy liver cells are gradually replaced by scar tissue.
As scar tissue accumulates, blood flow becomes restricted, and liver function may decline, affecting detoxification, protein production, metabolism, and bile processing.
Compensated vs decompensated cirrhosis
Doctors use the terms “compensated” and “decompensated” to describe where a patient is on the cirrhosis timeline—mainly based on whether major complications have already appeared. Portal hypertension often develops along the way and helps explain why some patients later move from one stage to the other.
- Compensated cirrhosis: the liver is damaged, but it retains enough functional reserve to perform its essential tasks. Symptoms may be mild.
- Decompensated cirrhosis: functional reserve is exhausted and can no longer maintain normal liver function, leading to overt complications. Common examples are ascites (fluid in the abdomen), hepatic encephalopathy (confusion from toxin buildup), and portal hypertensive bleeding (often from varices).
Portal hypertension and why it drives complications
As scarring increases, pressure rises in the portal vein system. This is called portal hypertension. It can lead to:
- Varices (swollen veins in the esophagus or stomach) that can bleed
- Ascites and leg swelling
- Higher risk of infections
- Kidney stress
Get a free online consultation
Get a free online consultation with a medical advisor to find out how stem cells would benefit your case.

Medical Advisor, Swiss Medica doctor
Common Causes and Risk Factors
Cirrhosis can come from different causes, but the logic is always the same: if the trigger continues, the liver keeps getting injured. This is why the first step in any treatment plan—before discussing regenerative options—is to identify the cause and bring it under control.
Long-term alcohol use can cause persistent inflammation and oxidative stress, which speeds up fibrosis. The risk increases with higher intake and longer duration. The most important step is complete alcohol abstinence, and many patients benefit from structured support such as counseling, medical supervision, and a clear relapse-prevention plan.
Chronic hepatitis B and C can damage the liver silently for years, which is why many patients are diagnosed only after fibrosis has already progressed. Antiviral treatment can help control the infection, slow further liver injury, and reduce the risk of complications, but existing scarring may not fully reverse—so regular monitoring remains an important part of long-term care.
Fatty liver disease and metabolic dysfunction (NAFLD/NASH)
Fatty liver disease, linked to obesity and insulin resistance, can progress to steatohepatitis and cirrhosis. The biggest protective factors are weight reduction (gradual and sustainable), better metabolic control, and long-term lifestyle changes. If the metabolic driver stays active, inflammation often continues.
Autoimmune and genetic conditions
Autoimmune hepatitis and cholestatic diseases can gradually lead to cirrhosis if they are not diagnosed and treated early. In some cases, genetic or metabolic disorders also play a role, which is why these patients often need a more individualized workup and long-term monitoring. Some patients also explore broader regenerative options, including stem cells for autoimmune disease, especially when immune-driven inflammation plays a role in liver damage.
Why Standard Treatments Have Limitations
Standard hepatology care is essential and should never be skipped. It does much more than “manage symptoms”: it targets the cause when possible and prevents complications that can become life-threatening. However, once fibrosis is advanced, standard treatment may not be enough to restore function, which is why some patients begin looking for additional supportive options.
What standard care does well
- Treat the cause (antivirals, abstinence programs, metabolic treatment, autoimmune therapy)
- Prevent and manage complications (ascites, infections, encephalopathy, varices)
- Monitor severity and transplant timing
What standard care often cannot do
Even with excellent care, advanced scarring does not reliably “reset” back to normal liver structure. Some patients remain stable for years, while others progress despite appropriate management. This gap—when the disease is controlled but function remains limited—is one reason regenerative approaches are considered as an add-on in selected cases.
Using Stem Cells for Liver Cirrhosis: How They Support Liver Repair
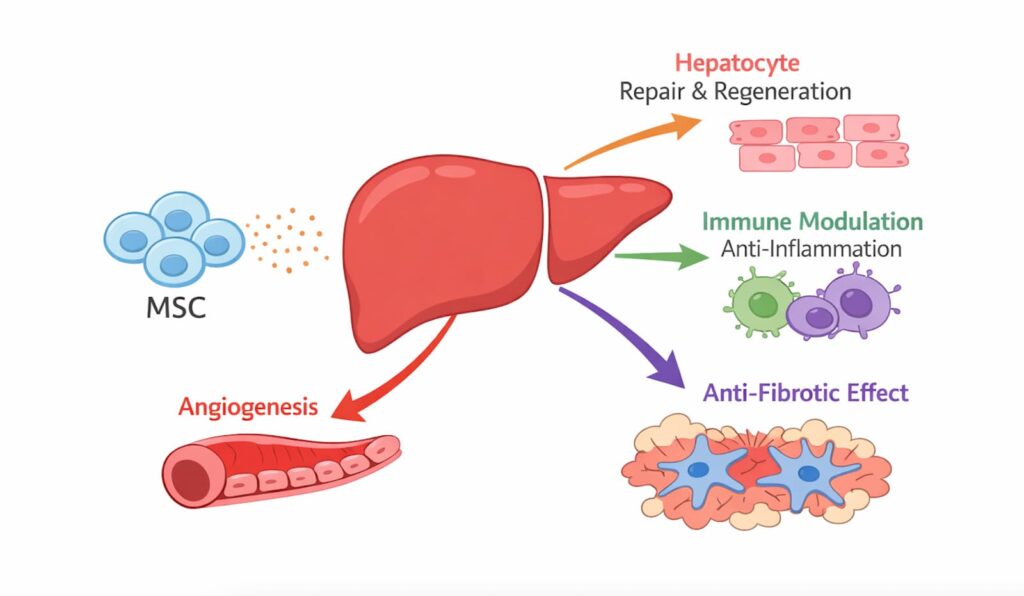
Stem cell therapy usually means regenerative cell-based support. The most widely used and studied option in liver programs is mesenchymal stromal/stem cells (MSCs). These cells are not meant to replace the liver. Instead, the goal is to use their biological signaling to support the body’s own repair processes.
How MSCs may support liver repair
Most proposed benefits relate to paracrine signaling. In simple terms, cells release signals that can:
- Reduce harmful inflammation
- Influence fibrosis pathways
- Support tissue remodeling and microcirculation
Can stem cells cure liver cirrhosis?
Evidence does not support guaranteed reversal for everyone. The realistic goal of liver cirrhosis treatment with stem cells is supportive improvement or stabilization in patients who are medically suitable for therapy, alongside standard hepatology care.
Stem Cell Therapy for Liver Cirrhosis in Clinical Trials and Research
Stem cell therapy for liver cirrhosis has been evaluated in a growing number of clinical trials, with the strongest and most consistent data coming from studies using MSCs.
Clinical research and meta-analyses have reported measurable improvements in liver function and disease severity in selected patients. These include increases in serum albumin levels and reductions in MELD and Child–Pugh scores, which are widely used indicators of liver synthetic function and prognosis.
From a safety perspective, published trials generally describe MSC-based therapy as well tolerated when treatment is performed under controlled medical conditions.
While stem cells for liver cirrhosis do not replace liver transplantation, research suggests they may help stabilize liver function, slow disease progression, and improve functional outcomes in appropriately selected patients.
Ongoing clinical trials continue to refine treatment protocols, dosing strategies, and patient selection criteria to better define long-term benefits.
Stem Cells for Liver Cirrhosis: What Types Are Used in Therapy?
At Swiss Medica, stem cell therapy for liver cirrhosis is based on MSCs, as they are the most studied and clinically appropriate option for chronic liver disease.
Why MSCs are used
MSCs are selected for their anti-inflammatory, immunomodulatory, and anti-fibrotic effects, as well as a favorable safety profile.
Cell sources used
- Umbilical and placental-derived MSCs are the primary source at Swiss Medica. These cells are obtained from donors after healthy childbirth, allowing consistent quality control.
- Bone marrow–derived MSCs are used in selected cases, depending on individual clinical indications.
Additional cell products
- Exosomes are MSC-derived microvesicles with bioactive molecules. Possess regenerative abilities and enhance the effect of stem cell therapy.
- Macrophage-based approaches focus on immune cells that control inflammation and tissue cleanup. Macrophage precursor cells circulate in the blood, then move to inflamed tissue and mature into macrophages. Depending on local signals, macrophages can either amplify inflammation or support repair and remodeling.
“Stem cell therapy” is an umbrella term. Treatment quality depends on the cell type, source material, and standardized preparation and quality-control procedures.
Explore the cells we use and our quality standardsTreatment Process at Swiss Medica
Stem cell therapy for liver cirrhosis at Swiss Medica follows a structured medical pathway focused on patient safety and individualized care.
Diagnostic evaluation and eligibility
Each patient undergoes a detailed review of diagnosis, disease stage, complications, prior treatments, and current medications. Laboratory results and imaging are assessed to confirm eligibility and potential risks.
Cell preparation and administration methods
Swiss Medica uses high-quality donor MSCs that have been carefully screened, tested for sterility, and checked for quality in our in-house laboratory.
Depending on the clinical plan, cells may be delivered either through an intravenous (IV) infusion or by a local injection into the targeted area.
Supportive therapies during the program
Stem cell therapy is combined with supportive care, including nutritional guidance, metabolic support, monitoring of fluid balance, and infection prevention. This integrated approach helps create conditions where regenerative therapy may have the greatest potential benefit.
What Improvements Can Patients Expect?
Stem cell therapy for liver cirrhosis is not a universal solution, but clinical research and practice suggest that some patients may experience functional improvements when therapy is used at an appropriate stage and combined with standard care. However, individual outcomes vary depending on disease stage, cause control, and overall health status.
Slower fibrosis progression
MSCs release bioactive substances that naturally stabilize the effects of body cells, thereby reducing excessive inflammation that leads to fibrosis.
Improved liver function test results (ALT, AST, bilirubin)
Laboratory markers such as ALT, AST, bilirubin, and albumin decrease after MSC-based therapy. These changes may reflect improved liver cell function and reduced inflammatory activity, although results are not uniform across all patients.
Increased energy, reduced fatigue, improved digestion
When liver function stabilizes, patients may notice better daily energy levels, reduced fatigue, improved appetite, and more stable digestion. These changes can have a meaningful impact on quality of life, especially when combined with nutritional support and complication prevention.
Patient from the UK—real experience
“Before coming to Swiss Medica, I was struggling with severe fatigue, weakness, brain fog, poor appetite, and overall low stamina—my daily life felt limited. After starting the program, my main goal became clear: to stabilize the condition and help my body regain strength and energy, improve digestion, and reduce the constant fogginess. I understand cirrhosis is complex, but even meaningful functional improvements and slowing progression would be a real win for me.”
You can find over 500 testimonials from Swiss Medica patients on our official YouTube channel.
Risks, Contraindications, and Safety Considerations in Stem Cell Therapy for Liver Cirrhosis
Safety is a critical factor in any regenerative therapy, particularly in patients with chronic liver disease.
Most patients tolerate MSC-based therapy well after eligibility screening, but cirrhosis can be unstable, and some people may temporarily feel more tired or weak during treatment due to their underlying condition. This is why we monitor patients closely and adjust the plan to prioritize stability.
Why advanced cirrhosis stages may respond differently
Advanced or unstable cirrhosis may limit the body’s ability to respond to regenerative signals. Severe portal hypertension, recurrent infections, kidney dysfunction, or frequent decompensation episodes can reduce potential benefit and increase procedural risk.
For this reason, patient selection and timing are essential.
Safety protocols at Swiss Medica
At Swiss Medica, safety is not an “extra” step—it is the foundation of our liver cirrhosis program.
We prioritized safety through:
- Comprehensive pre-treatment evaluation to confirm diagnosis, stage, comorbidities, and current risks before any therapy begins
- Strict eligibility and contraindication screening, including assessment for infections, unstable decompensation, and oncology-related risks
- In-house laboratory and cryobank support, with controlled cell handling, traceability, and sterility standards
- Quality control checks of cell products (including sterility and viability confirmation) before administration
- Individualized dosing and treatment planning, adjusted to the patient’s condition, tolerance, and clinical response
- Continuous medical supervision during the program, with regular monitoring and the ability to modify the plan if warning signs appear
If you’d like to learn more about how we prioritize safety, you can read about Swiss Medica’s in-house laboratory and the quality-control steps used in cell preparation.
Read the full overviewWho Is a Suitable Candidate for Stem Cell Therapy for Liver Cirrhosis?
At Swiss Medica, we review each case individually. The stage of cirrhosis, overall stability, and whether the underlying cause is under control help us understand what level of benefit is realistic and how to keep the program safe and effective.
Eligibility Factors
Our program considers patients with:
- Compensated or early decompensated cirrhosis
- Stable overall condition (no uncontrolled bleeding, no rapidly worsening organ failure)
- Ability to follow a structured plan and attend follow-up monitoring
Who may not qualify for liver cirrhosis treatment with stem cells
- Active malignancy or strong suspicion needing urgent evaluation
- Severe unstable decompensation (recurrent bleeding, uncontrolled encephalopathy, severe kidney failure not stabilized)
- Ongoing alcohol use or inability to follow essential monitoring and treatment
- Situations where urgent liver transplant eligibility evaluation should be prioritized
Complementary Therapies That Support Liver Repair After Stem Cell Therapy for Liver Cirrhosis
Stem cell therapy is only one part of the program. The best results usually come when the liver is not being “hit” again by the same triggers, and the body stays stable while recovery signals are working.
That’s why we recommend combining regenerative therapy with supportive care that helps protect liver function and reduce setbacks.
- Cause control: continue the core plan (antivirals, alcohol cessation support, metabolic control, and autoimmune therapy if prescribed).
- Nutrition support: adequate protein and calories (as advised), correction of deficiencies only if confirmed by labs.
- Infection prevention (a cirrhosis-related risk): prompt treatment and follow-up if there is a history of infections such as spontaneous bacterial peritonitis (SBP).
- Encephalopathy prevention: physician-guided lactulose/rifaximin when needed; avoid sedatives unless essential.
- Lifestyle basics: gentle activity to reduce muscle loss, good sleep, strict avoidance of alcohol and “detox” supplements.
Stem Cell Therapy for Liver Cirrhosis vs Other Innovative Treatments
Patients may encounter innovative options for cirrhosis, but they differ in purpose and level of clinical use. The table below compares these approaches and highlights how stem cell transplant for liver cirrhosis at Swiss Medica is positioned as a structured regenerative program.
| Method | What it aims to do | Main limitation | Why stem cell therapy can be a stronger option |
| Anti-fibrotic investigational drugs | Slow or block fibrosis pathways | Many are experimental with limited access | Stem cell therapy aims to support the liver through immune and inflammation control plus tissue-support signals |
| Plasma exchange | Temporarily reduce toxins and inflammatory mediators | Short-term stabilization, not regeneration | Stem cell therapy is designed for longer-term functional support, not only temporary detox |
| Regenerative peptides | Short chains of molecules marketed to “support recovery” in the body | Evidence for cirrhosis outcomes is inconsistent | Stem cell therapy uses a more defined approach with controlled preparation and medical supervision, rather than variable supplement-like protocols |
| Liver support systems | Temporary detox support (“bridge”) | Not a cure; temporary | Stem cell therapy is a planned program for eligible patients aimed at improving stability and daily functioning over time |
Availability and Cost of Stem Cell Therapy for Liver Cirrhosis
Searching for new solutions to manage cirrhosis and improve quality of life is a common situation in a patient’s life. However, the chosen treatment may be available only abroad, especially if it is relatively new.
Where can you get stem cell treatment for cirrhosis?
Access to stem cell therapy depends on the country and its regulations. For example, stem cell treatments for liver cirrhosis in the USA are limited to clinical trials.
In other countries, availability may be broader, but safety standards, cell processing requirements, and clinical oversight can vary significantly—so it’s important to evaluate each provider carefully.
Swiss Medica, in Serbia, provides stem cell therapy within a regulated medical program that includes structured evaluation, laboratory oversight, and physician supervision. This makes it an option for international patients seeking regulated regenerative treatment outside clinical trials.
The cost of stem cell therapy for liver cirrhosis depends on disease severity, diagnostics, length of stay, and supportive care needs. Our program costs range from €7,000 to €31,000.*
* Prices are indicative, based on 2026, and may vary with condition severity and cell quantity required.
Why Patients Choose Swiss Medica
For many international patients, choosing a stem cell clinic comes down to medical oversight, lab control, and consistent daily monitoring. At Swiss Medica, these are built into the treatment plan:
- We have worked in regenerative medicine since 2011.
- A multidisciplinary team collaborates on each case within one coordinated plan.
- In-house A-grade laboratory and cryobank ensure safety through strict cell control.
- All-inclusive stay: the program cost typically includes accommodation, meals (including special dietary needs), services for one accompanying person, airport transfers, and interpreter support—especially helpful for international patients.
- Hotel-like environment with careful staff and a home-like atmosphere in our hospital.
- Focused attention: the doctor-to-patient ratio is intentionally kept low (around 3–4 patients per doctor).
How to Apply for Stem Cell Therapy for Liver Cirrhosis
The process begins with an initial consultation to evaluate the diagnosis and current condition. If the case is suitable, we explain the program clearly—what it includes, how long it takes, and what to expect day by day.
When you arrive, our doctors run on-site diagnostics to confirm safety and fine-tune your individual plan.
Contact us
If you’re living with cirrhosis and considering stem cell therapy, you can reach out to our medical team for a consultation. We’ll review your case and explain whether this approach may be suitable, what results are realistic, and what safety checks are involved—so you can make an informed decision at your own pace.

Medical Advisor, Swiss Medica doctor
Frequently Asked Questions
1. Can a stem cell transplant for liver cirrhosis replace a liver transplant?
Treatment of cirrhosis with stem cells is not meant to replace a liver transplant. For some patients, it may help stabilize liver function or slow progression, but it does not eliminate the importance of transplant assessment if your doctor recommends it.
2. How long do results last after liver cirrhosis treatment with stem cells?
The duration of effect varies from patient to patient. While some early signs of improvement can appear in weeks, the peak effect is usually seen at 1.5–2 months, with further gradual progress possible. Long-term results depend strongly on disease stage, control of the underlying cause, nutritional status, and follow-up visits.
3. Is the therapy safe for advanced cirrhosis?
Advanced decompensated cirrhosis carries higher risks regardless of treatment type. In patients with severe instability, active infections, or significant kidney failure, stem cells for liver cirrhosis may not be appropriate. Careful medical evaluation is essential to determine whether potential benefits outweigh risks in advanced stages.
4. Can I travel with cirrhosis?
If stem cell therapy is not available where you live (as can be the case for stem cell treatment for liver cirrhosis in the USA, UK, and some European countries), you may come across clinics abroad that offer it. For patients with stable cirrhosis, travel can sometimes be possible—but it requires careful preparation. Before making plans, speak with your treating doctor to make sure flying and traveling are safe for you.
List of References:
Wang H, Yao W, Wang Y, Dong H, Dong T, Zhou W, Cui L, Zhao L, Zhang Y, Shi L, Jiang Y. Meta-analysis on last ten years of clinical injection of bone marrow-derived and umbilical cord MSC to reverse cirrhosis or rescue patients with acute-on-chronic liver failure. Stem Cell Res Ther. 2023 Sep 23;14(1):267. doi: 10.1186/s13287-023-03494-2.
Lu, W., Qu, J., Yan, L. et al. Efficacy and safety of mesenchymal stem cell therapy in liver cirrhosis: a systematic review and meta-analysis. Stem Cell Res Ther 14, 301 (2023). https://doi.org/10.1186/s13287-023-03518-x
Xie, Y., Zhang, Z., Pan, Y. et al. Stem cells therapies for liver diseases: for current practice and future goals. Hepatol Int 19, 1051–1076 (2025). https://doi.org/10.1007/s12072-025-10835-1
Liu Y, Dong Y, Wu X, Xu X, Niu J. The assessment of mesenchymal stem cells therapy in acute on chronic liver failure and chronic liver disease: a systematic review and meta-analysis of randomized controlled clinical trials. Stem Cell Res Ther. 2022 May 16;13(1):204. doi: 10.1186/s13287-022-02882-4.
MD, Pediatrician, Regenerative Medicine Specialist











