COPD stands for ‘chronic obstructive pulmonary disease’. It’s an umbrella term that includes several lung diseases that affect a person’s ability to breathe, causing coughing and fatigue. Most commonly, these are emphysema and chronic bronchitis. Chronic asthma should not be confused with COPD, but it can sometimes coexist with it.
According to the World Health Organization, COPD is the third leading cause of death in the world, right behind heart problems and cancer. What is the medical treatment for COPD? Unfortunately, as of now, there is no cure for COPD. As time passes, the symptoms usually continue to progress, lowering the quality of life and causing additional medical problems.
Yet while COPD cannot be reversed completely, several different COPD treatment options may help to manage the symptoms and slow down the progression of this disease.
The following list is for reference only. To determine the best treatment for COPD, consult a medical professional.
Medications for COPD
Treatment for COPD patients typically involves a combination of medications that help manage symptoms and slow the progression of the disease.
Bronchodilators: types and how they work
Bronchodilators are inhaler-type medicines that relax and widen the airways. This way, breathing becomes easier, which alleviates the symptoms. There are different types of bronchodilators used as a treatment for COPD cough.
- Short-acting bronchodilators are usually used before physically taxing activities or during flare-ups (also called exacerbations) to ensure short-term relief. These are used ad hoc and aren’t suitable for constant use throughout the day. Nevertheless, they are an effective treatment for COPD exacerbations.
- Long-acting bronchodilators are similar to short-acting ones in what they do. However, these are aimed at continuous daily use and are employed when flare-ups are too frequent or short-acting bronchodilators are ineffective.
Inhaled corticosteroids: their role in COPD treatment
Corticosteroids are man-made anti-inflammatory drugs that closely resemble cortisol, a hormone that is produced by the human body naturally. Usually, they are used alongside long-acting bronchodilators if the latter is not enough as a treatment for COPD exacerbations.

Other medications: antibiotics, mucolytics, and oxygen therapy
- Antibiotics can be used when COPD symptoms are worsened by respiratory infections, such as pneumonia or bronchitis. However, the overuse of antibiotics carries additional risks, so they cannot be used for long-term COPD treatment.
- Mucolytics are drugs that help break up the mucus in the lungs, so coughing it out becomes easier. These medications help to ease the flare-ups and reduce the impact that COPD has on the patient’s quality of life.
- Oxygen therapy consists of delivering oxygen to the patient’s lungs via special devices. A person may need oxygen therapy if the levels of oxygen in their blood are too low because of COPD. The therapy may be conducted both in ambulatory settings and at home, although it’s always best to consult a professional before engaging in any COPD chronic bronchitis treatment.
Pulmonary Rehabilitation
Pulmonary rehabilitation is aimed at alleviating symptoms and slowing down the progression of COPD. It includes physical exercises, breathing practices, and education on the nature of the disease and the function of the lungs. This COPD treatment algorithm is usually created and supervised by medical professionals.
Benefits of pulmonary rehabilitation for COPD patients
Pulmonary rehabilitation may alleviate the symptoms of COPD, help the patient breathe easier, make them more equipped to deal with their particular health situation, teach them to relax more effectively, and raise their overall quality of life.
Components of a pulmonary rehabilitation program
- Aerobic and strength exercises. Body training and conditioning result in better breathing and the ability to do more tasks without shortness of breath and flare-ups. It can also compensate for muscle loss that might be associated with COPD.
- Breathing exercise. Also called inspiratory muscle training (IMT), this involves the specific muscles that are used in the process of breathing.
- Education. The patients are informed about their lung problems, the best treatment for COPD in their specific situation, the necessary COPD treatment medications, and when and how to take them.
How pulmonary rehabilitation improves quality of life
After rehabilitation, a person is more equipped physically and mentally to manage the symptoms of COPD. They can understand their situation better and don’t feel helpless in the face of their affliction. This lowers anxiety and allows patients to take better care of themselves. Therefore, this results in a higher quality of life.
Get a free online consultation
Please, contact our medical advisor to discuss your health condition with a specialist in regenerative medicine. You can also leave your contact details for a callback. It is free and confidential.
Lifestyle Changes and Self-Care
Outside of professional medical help, the best treatment for COPD revolves around a healthy lifestyle and taking good care of yourself and your specific needs.
Smoking cessation: importance and strategies
Smoking is one of the foremost factors that develop and worsen COPD. The chemicals in tobacco products weaken your lungs’ defense against infection. Smoking cessation helps to slow the progression of the disease. It is even considered to be the best treatment for COPD.
The variety of smoke cessation aids and methods is beyond the scope of this article, but you should consider the main 3 strategies.
- Self-care. A person can stop smoking without outside help. Concentrate on finding more publicly available information and self-care approach, rather than force of will.
- Group therapy. Withdrawing from an addiction is difficult, and it might be easier if you have support and understanding. Finding a group of like-minded people can increase your motivation and results.
- Clinical help. You should always ask for help from medical professionals, who will create the best program tailored to your needs.
Exercise and physical activity: benefits for COPD patient
Higher levels of physical activity significantly improve the quality of life by strengthening breathing muscles, improving oxygen intake, and overall contributing to higher capability and mobility. Consider introducing more intensive aerobic training to your daily regimen.
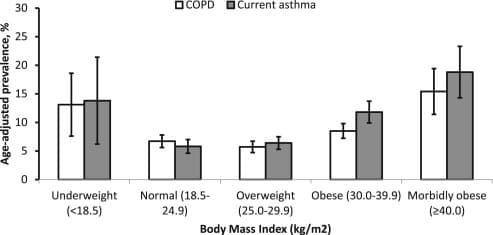
Nutrition and maintaining a healthy weight
Obesity correlates with more frequent severe flare-ups and higher mortality rates from COPD. Changing diets or consulting a dietician is advised for COPD patients with a high BMI.
Managing stress and mental health
Living with COPD may be challenging for a person’s mental state. The prospect of early death, the inability to carry out everyday tasks for fear of a flare-up—all of this is scary and anxiety-inducing. Attending therapy and support groups is a way to combat that.
Oxygen Therapy
Indications for oxygen therapy in COPD
Oxygen therapy is mostly used in 2 cases.
- Ad hoc, to manage an acute flare-up.
- Constantly, if the oxygen levels in a patient’s blood are consistently low.
Monitoring oxygen levels and compliance with therapy
To check the levels of oxygen in the blood, you need an oximetry device. A quick and painless way to do this is to use a pulse oximeter. The number that it shows is a value of oxygen saturation. If it goes lower than 95%, you may need to make an appointment with your doctor.

Types of oxygen delivery systems
Usually, oxygen comes to the patient from the nasal tube that is attached to a device. There are three types of devices.
- Oxygen concentrator: a device that separates the oxygen from the nitrogen in the room air.
- Liquid oxygen system: stores oxygen in the form of a liquid and allows it to evaporate, so it becomes breathable for the patient.
- Compressed gas system: oxygen is stored in high-pressure tanks and released as needed.
Stem Cell Therapy
Stem cell therapy is a form of advanced COPD treatment that uses stem cells to improve the activation of a patient’s tissues and enhance the regenerative capacity of the damaged parts of a lung. It’s a relatively new treatment for COPD.
How stem cell therapy works for COPD treatment
Stem cell therapy for COPD and chronic bronchitis involves the use of stem cells to repair damaged lung tissue. These cells can change into any cell in the body—the process is called differentiation.
At Swiss Medica, we administer mesenchymal stem cells (MSC) intravenously and via inhalation. Additionally, during inhalation, we deliver exosomes derived from MSC cells.
When cells reach the lungs, they start to cover the damaged areas, enhancing the repair of the structure. The lungs become more functional, making exacerbations rarer. Stem cells also have anti-inflammatory properties, which can clear airways for those with chronic bronchitis. This makes them the best treatment for COPD in some regards.
Surgical Interventions
When the lungs are severely damaged, a medical professional may advise COPD patients to undergo a more radical surgical treatment.
Lung volume reduction surgery (LVRS)
LVRS (or lung volume reduction surgery) involves removing the damaged part of the lung to allow the remaining lung to work better. LVRS is not a one-size-fits-all solution because the success of the operation depends on the condition of the patient, their age, and whether they are smokers.
Lung transplantation: considerations and eligibility criteria
When the lung is deemed to be beyond saving, it will often need to be replaced. To be eligible to receive a lung transplant, a person needs to meet the criteria established by the International Society of Heart and Lung Transplantation. A medical team will help you know if you are eligible, but the rough outlines are:
- Having an end-stage lung disease.
- The ability to live through the transplantation.
- High likelihood of surviving 5 years after the transplant.
- There is a high risk of death in 2 years related to lung disease.
However, please note that any decisions regarding COPD treatment should be taken only after consulting with a professional, as the circumstances and conditions vary.
Managing Exacerbations
A flare-up is a sudden worsening of COPD symptoms. It may last up to 2 days, but it may also get more severe or not go away. It can get counteracted, but it is important to know when and how.
Recognizing and responding to COPD exacerbations
How do you recognize that you are having a flare-up? See if you experience any of those:
- Increased cough;
- Problems with sleep;
- Inability to take a deep breath;
- Louder breathing;
- Get tired more quickly.
Treatment options during exacerbations
If you find yourself in the middle of the flare-up, do not panic. Take the medication that your doctor has recommended to you, whether it is inhaled medicine, home oxygen therapy, or antibiotics. You may also try breathing exercises such as pursed lip breathing.
If the symptoms persist after 48 hours or if the symptoms are getting worse despite taking medicine, seek professional help.
Importance of follow-up care after exacerbations
COPD is not a seasonal flu that goes away quickly. Even after the exacerbation ends, it’s important to stay cautious. Make sure to see your doctor for a follow-up appointment. If you do not change anything in your lifestyle, the flare-up is likely to happen again.
Unfortunately, COPD keeps getting worse over time, severely impacting the quality of life and sometimes leading to death. Contact a healthcare provider to determine your new treatment for COPD and manage the condition early on.
Contact us
Get a free online consultation to learn about the expected results of stem cell therapy for your case, what is the cost of the treatment, and its duration.
List of References:
Soriano, J. B., & Lamprecht, B. (2012). Chronic obstructive pulmonary disease: a worldwide problem. The Medical Clinics of North America, 96(4), 671–680. https://doi.org/10.1016/j.mcna.2012.02.005
Tønnesen P. (2013). Smoking cessation and COPD. European respiratory review: an official journal of the European Respiratory Society, 22(127), 37–43. https://doi.org/10.1183/09059180.00007212
García-Gómez, L., Hernández-Pérez, A., Noé-Díaz, V., Riesco-Miranda, J. A., & Jiménez-Ruiz, C. (2019). SMOKING CESSATION TREATMENTS: CURRENT PSYCHOLOGICAL AND PHARMACOLOGICAL OPTIONS. Revista de investigacion clinica; organo del Hospital de Enfermedades de la Nutricion, 71(1), 7–16. https://doi.org/10.24875/RIC.18002629
Lan, C. C., Chu, W. H., Yang, M. C., Lee, C. H., Wu, Y. K., & Wu, C. P. (2013). Benefits of pulmonary rehabilitation in patients with COPD and normal exercise capacity. Respiratory care, 58(9), 1482–1488. https://doi.org/10.4187/respcare.02051
Hanson, C., Rutten, E. P., Wouters, E. F., & Rennard, S. (2014). Influence of diet and obesity on COPD development and outcomes. International journal of chronic obstructive pulmonary disease, 9, 723–733. https://doi.org/10.2147/COPD.S50111
Ubolnuar, N., Tantisuwat, A., Thaveeratitham, P., Lertmaharit, S., Kruapanich, C., Chimpalee, J., & Mathiyakom, W. (2020). Effects of pursed-lip breathing and forward trunk lean postures on total and compartmental lung volumes and ventilation in patients with mild to moderate chronic obstructive pulmonary disease: An observational study. Medicine, 99(51), e23646. https://doi.org/10.1097/MD.0000000000023646
Rochester, C. L., Alison, J. A., Carlin, B., Jenkins, A. R., Cox, N. S., Bauldoff, G., Bhatt, S. P., Bourbeau, J., Burtin, C., Camp, P. G., Cascino, T. M., Dorney Koppel, G. A., Garvey, C., Goldstein, R., Harris, D., Houchen-Wolloff, L., Limberg, T., Lindenauer, P. K., Moy, M. L., Ryerson, C. J., … Holland, A. E. (2023). Pulmonary Rehabilitation for Adults with Chronic Respiratory Disease: An Official American Thoracic Society Clinical Practice Guideline. American journal of respiratory and critical care medicine, 208(4), e7–e26. https://doi.org/10.1164/rccm.202306-1066ST
Holland, A. E., Cox, N. S., Houchen-Wolloff, L., Rochester, C. L., Garvey, C., ZuWallack, R., Nici, L., Limberg, T., Lareau, S. C., Yawn, B. P., Galwicki, M., Troosters, T., Steiner, M., Casaburi, R., Clini, E., Goldstein, R. S., & Singh, S. J. (2021). Defining Modern Pulmonary Rehabilitation. An Official American Thoracic Society Workshop Report. Annals of the American Thoracic Society, 18(5), e12–e29. https://doi.org/10.1513/AnnalsATS.202102-146ST
Medical Advisor, Swiss Medica doctor








